 We hear a lot about vitamins and minerals such as B12, folate, magnesium, vitamin C, and so on, but there seems very little talk these days on the importance of dietary lecithin and choline. Are you consuming an adequate amount of acetylcholine, or other phospholipids? The odds are that you are not.
We hear a lot about vitamins and minerals such as B12, folate, magnesium, vitamin C, and so on, but there seems very little talk these days on the importance of dietary lecithin and choline. Are you consuming an adequate amount of acetylcholine, or other phospholipids? The odds are that you are not.
A little bit about choline
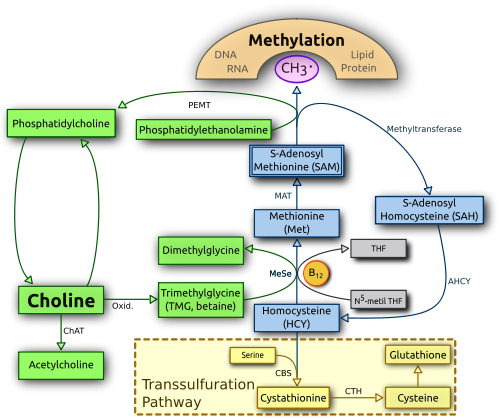
The human body produces choline by methylation of phosphatidylethanolamine (from dietary sources such as lecithin and others) to form phosphatidylcholine in the liver by the PEMT enzyme. Phosphatidylcholine may also be consumed in the diet or by supplementation. Choline is oxidized to betaine which acts as an important methyl donor and osmolyte.
For those wanting to see how this relates to the methylation cycle, below is a nice graphic (courtesy of Wikipedia).
It is well known that magnesium deficiency is widespread (57% of the population does not meet the U.S. RDA according to the USDA), but the numbers for choline deficiency are even more shocking.
According the National Health and Nutrition Examination Survey (NHANES) in 2003-2004, only about 10% of the population have an adequate intake of choline. This means about 90% of the population consumes a diet deficient in choline. Furthermore, those without an adequate intake of choline may not have symptoms.
Along with folate and B12 deficiency, inadequate consumption of choline can lead to high homocysteine and all the risks associated with hyperhomocysteinaemia, such as cardiovascular disease, neuropsychiatric illness (Alzheimer’s disease, schizophrenia) and osteoporosis. Inadequate choline intake can also lead to fatty liver or non-alcoholic fatty liver disease (NAFLD).
The most common symptoms of choline deficiency are fatty liver and/or hemorrhagic kidney necrosis. Consuming choline rich foods usually relieve these deficiency symptoms. Diagnosing fatty liver isn’t as simple as running ALT and AST since nearly 80% of people with fatty liver have normal levels of these enzymes according to a population study published in the journal Hepatology. In fact, in an experiment, 10 women were fed a diet low in choline. Nine developed fatty liver and only one had elevated liver enzymes.
For those who are genotyped by 23andMe, there is a SNP (rs7946) related to NAFLD you can look at in the PEMT gene called PEMT G523A (V175M). Caucasians with nonalcoholic fatty liver are more likely to carry the rs7946 (T), with the effect being most pronounced for rs7946(T;T) genotypes. [PMID 16051693]
If you are genotyped by 23andMe, make sure you are logged in to 23andMe and you will see your results for this SNP.
Choline, the nervous system, and the heart
Despite it’s role in the CNS and stimulating parasympathetic activity, there is very little info about choline and mental illness. However, in a large population-based study published in The American Journal of Clinical Nutrition, people with higher blood levels of choline had lower levels of anxiety – however, levels of choline did not correlate with depressive symptoms.
Despite the lack of studies, it has been clinically observed that supplementing Lecithin or putting patients on a Lecithin rich diet can lower levels of anxiety, help the nervous system by establishing balance between sympathetic and parasympathetic, and even manage cardiac dysrhthmias. The Milner Acetylcholine Protocol (MAP) uses lecithin to manage cardiac dysrhthmias.
Phospholipids and the cell membrane
The fundamental building blocks of all cell membranes are phospholipids. Lecithin consists of phospholipids such as phosphatidylcholine, phosphatidylethanolamine, phosphatidylinositol, Phosphatidic acid, other minor phospholipids and glycolipids. About 50% of the mass of most cell membranes are composed of phospholipids. The plasma membranes of cells also contain glycolipids and cholesterol – which correspond to about 40% of the total lipid molecules. Adequate intake of phospholipids and glycolipids is important for the integrity of the cell membranes. Lecithin contains a balanced amount of phospholipids and glycolipids.
Phospholipid supplementation has also been shown to help with mitochondrial dysfunction in patients with diseases such as Chronic Fatigue Syndrome, chronic Lyme Disease, Fibromyalgia, and Gulf War Illness. Fatigue reduced about 40% in Chronic Fatigue Syndrome patients after lipid replacement therapy (supplementing phospholipids) according to the Journal of Chronic Fatigue Syndrome.
Adequate intake of choline and choline-rich foods
Adequate intake of choline varies by age. Here is a table by CholineInfo.org.
Adequate Intake (AI) levels for choline are:
Population |
Adequate Intake (AI)
|
| Infants:(0-6 months) (7-12 months) |
125 milligrams 150 milligrams |
| Children:(1-3 years) (4-8 years) (9-13 years) |
200 milligrams 250 milligrams 375 milligrams |
| Adolescents:(14-18 years) | 400 milligrams (Females) 550 milligrams (Males) |
| Adults:(19 and older) | 425 milligrams (Females) 550 milligrams (Males) |
| Pregnant women | 450 milligrams |
| Breastfeeding women | 550 milligrams |
CholineInfo.org also has a very nice graphic showing the best sources of choline. According to their chart, beef liver and egg are by far the best sources for lecithin with modest amounts in lean beef, chicken breast, cod, wheat germ, and cauliflower.
Unfortunately, not all nutrition data is the same, and for the sake of comparison, below is what Wikipedia lists as high choline foods.
Since cooking eggs at high temperatures destroys the choline content, it’s best to cook the egg so the yolk is runny to preserve lecithin content. For people without egg allergies, properly cooked eggs is one of the best sources of lecithin.
In presence of an egg allergy, consuming liver or supplementing with sunflower lecithin may be the best options to ensure an adequate intake of choline. Sunflower lecithin may be a better source for lecithin than soy because unlike soy lecithin, sunflower lecithin is never derived from GMO crops. Also, soy is generally more allergenic than sunflower, so soy lecithin could potentially provoke unwanted effects in sensitive individuals.
Acetylcholine, phospholipids, autoantibodies, and a word of caution
Acetylcholine and antiphospholipid autoantibodies are seen in various autoimmune and chronic illnesses. It is well know that with Myasthenia Gravis, patients most commonly have autoantibodies against nicotinic acetylcholine receptor (nAChR). A large number of CFS patients may have acetylcholine receptor antibodies according to a study published in the International Journal of Molecular Medicine.
Dysautonomia and POTS can also be associated with autoantibodies against acetylcholine receptors. Mayo medical laboratories has a very comprehensive Autoimmune Dysautonomia Evaluation lab test that tests for autoantibodies against acetylcholine receptors and much more.
Antiphospholipid Syndrome (or Hughes syndrome) is an autoimmune condition that can lead to hypercoagulation and blood clots. Conditions such as Lupus, Sjogren’s syndrome, Chronic Fatigue Syndrome, and Fibromyalgia are often associated with antiphospholipid antibodies. Antiphospholipid antibodies can even develop in presence of chronic infections such as Hepatitis C, Syphilis, Chlamydia pneumoniae, EBV, HHV-6, Lyme disease, mycoplasma, Q Fever, and many other infections. Antiphospholipid syndrome can be tested for with LabCorp’s Thrombotic Risk Profile.
At this time there is insufficient evidence to determine if supplementing lecithin would be beneficial or harmful for those with acetylcholine receptor autoantibodies or antiphospholipid syndrome. More clinical research is needed to understand how lecithin supplementation influences the various autoimmune processes that may exist in these patients.
Whether you are a health expert with experience utilizing choline rich foods or lecithin supplements to treat chronic illness, or a patient using choline to promote your own health, please share your experience below.
Basolateral apical polarity and rear/front polarity are polarities determined by enzyme expression and location in cellular entities which promote epithelial and lumen tissue stability in the instance of basolateral polarity and which determine chemotaxis patterns with regard to rear/front polarity. Confluence is the ability of cellular entities to inherently sense when they have encountered tissue or structure over a percentage of the cellular surface using ligands that attach the cytoskeleton to external tissue or structure and using cellular/cellular junctions and proteins such as gap junction proteins. Confluence involves P21, P27, and P53 to impose tissue competent growth inhibition and chemotaxis inhibition while Hippo, Yap, Tax, Lat1 and Lat2 are mitotic signals involved confluence most centrally. The factors present in this information typically result in escape from confluence or escape from tissue stability imposed growth and chemotaxis inhibition.
An inducible version of a particular enzyme which uses Ca2+, for instance, causes strong gradients of Ca2+ from solid structure of physiology that can change systemic chemotaxis patterns for monocytes and result in patterns of condition advancement observed in pathology. Sirt1 overactivation is common modality linked to escape from senescence, although this can be differentially directed toward different outcomes if Dbc1 displaces Nad+ from the nudix homology domains that are exhibited in about 80,000 proteins in biology as a environmental modality of regulating biology.
Nad+ is interesting to understand because sparse, dense and very dense (H2e1p)- lakes span the universes and exhibit networks that include nearest neighbor (H2e1p)- carrying enzymes, proteins, tissue, molecules and biologically activity factors, while interacting at 30,000 times the velocity of light. Comprise, possibly, are interact networks that continuously emit influence, receive feedback and guide outcomes toward those which sustain, stabilize and support the status quo, while such adjudicative interactions potentiate also the emergence of competing outcomes in other eras which then impose deterministic influence on the status quo. This is why methylene cysteine below 6 or 7 um/L, access to stable nutrition, accesses to stable housing, access clean and stable water supplies, economic stability, social stability, education, social development, and other factors are so important in their ability to prevent competing outcomes in other eras from causing massive destabilizing of vital being, health, cognition and other aspects of the Human experience.
Carriers of (H2e1p)-, thus, operate in synapse that includes + or oxidized phase, as in Nad+, exist as NadH in the reduced phase, while also are exhibited as the molecule NAD although in biology, unless involved in another molecular configuration, the oxidized and reduced versions are most mentioned in the information and while NAD is at least mentioned in the research information. There are numerous other carriers of (H2e1p)-. The synapse between NADH oxidized (H2e1p)- and NAD+, including fluorescence and e eV- released when (H2e1p)- is oxidized from NADH in particular, exists as interactive statuses that provide influence, power, translatable influence into energy molecules, and even mechanical force, each of which assist in powering biology.
(H2e1p)- can be derived from paramagnetic and quantum spin liquid networks that move e-, nutritional pathways that provide carriers and sources of energy molecules and (H2e1p)-, lithium and Sodium which have high vapor pressure and allows them to siphon (H2e1p)- from networks of other element molecules harboring (H2e1p)-, along with other more controversial vectors which are confirmed in some instances and in other instances continued to be debated such as Human rubisco, Human pigment synthesis of energy and even phonons which involve sound’s ability to produce energy along with substantia nigra in which neurons generate energy from interactions in fields of influence in the universe, some of which have not been conclusively ascertained. Darkening of the substantia nigra are linked to development of coordinated movement in early development and deterioration of substantia nigra in neurons are linked to impaired coordination of movement.
Diminishing pH levels are linked with cellular entities increasing the protein content of extracellular exosomes while increasing the absorption of exosomes by cellular entities, explaining an important link between acidity in development of pathology in the microenvironment, particularly oncology.
The mysteries continue to reveal themselves, important info
The reason that glycolysis is not preferred over oxidative phosphorylation and electron transport pathway include that glycolysis is inefficient at producing ATP from glucose, mitochondrial interaction with organelles and structure is regulated by level of Ca2+ obtained from the interaction partner causing a linking of ATP production directly to the status of the organelle partnered with mitochondria, mitochondria interaction directly with cytosol/cytoplasm derives an expansive resource partner for sterol, glucose, Ca2+, and other factors, potentiating overproduction or dysregulated production of ATP which can cause over activation of ‘ases’ such as ATPase, which can cause subsequent overactivation of phosphate (ADP, ATP, AMP, and linked metabolites, etc) availability for kinase overactivation, these can cause GSK3B activation, g protein coupled receptor activation, S1P receptor activation, and cause enhanced resilience to apoptosis signaling.
Choline kinase is hyperactivated when PEMT is inhibited, this causes the cdp choline pathway to become hyperactivated in production of unenriched diminished DHA/Arachidonate/omega-3 fatty acid phosphatidylcholine along with overproduction of ATP attachment to choline as phosphocholine, and overproduction of S1P. Depletion of S1P by S1P lyase is a major therapeutic and immunological resistance pathway. Hyperproduction of phosphocholine provides substrate for proteolysis that release the ATP for proteolysis and systemic cellular level availability while also producing available of choline for hyperactivation of choline kinase, and while hyperactivation of cdp choline pathway is an allergen, xenobiotic and toxicity response that diminishes plasticity and causes utilization of methyltransferase which compete with Pemt for resources.
Phosphocholine is an allpurpose substrate for pathology and vectors that cause pathology including hyperactivation of resiliency signaling, while also being a subclinical activator of the complements immunological system and while also being able to directly activate platelets.
Inhibition of glycolysis by P53 when Pemt is diminished in availability and function also results decreased acetyl CoA which prevents choline from being stored as acetyl choline by choline acetyltransferase, enhancing the cycle of choline direction toward the cdp choline pathway.
The most intricate perspective in this regard is that inhibition of PEMT increases methylene cysteine (clinically hcy) which performs as inherent apoptosis signal that cause release of multiple apoptosis factor such as cytochrome C and others, requiring resilience signaling to be increase to counteract massive levels of apoptosis that emerge when Pemt is inhibited, although Pemt1 is naturally regulated in this regard by Pemt2 which emerges at conclusion of gestation. Methylene cysteine above 6 or 7 um/L and s adenosyl methylene cysteine above 0.012 um/L begin to cause clinical levels of apoptosis signaling, sequesters electrons from tissues, sequesters electrons of carriers of (h2e1p)-, sequesters electrons from biological active proteins/enzymes, and begins to cause a reliance upon major anatomical structures, enzymes, ion channels, molecules, adventitia and buffering system to maintain background pH at its optimal levels near, about or at pH 7.4.
Pemt moves CH3, exhibiting Carbon, 2 Hydrogens as H1e1p and 1 hydrogen as (H2e1p)- into cellular membranes, packing cellular membranes and tissues with (H2e1p)- the molecule integrally enabling stars to shine. This packing of membrane hydride enables tissues, structure and other factors to promote a background pH near, about or at pH 7.4 while also providing a source of (H2e1p)- that can be mined to provide (H2e1p)- integrated into carriers such as FAD, FADH2, NAD(H), NADP(H), and other factors which are used by the electron transport pathway in mitochondria efficiently, and with substantial regulation, to produce ATP. Removal of the electron in (H2e1p)- or carriers of (H2e1p)- is characterized as “protonation” because Hydrogen directly or indirectly since (h2e1p)- becomes distributed canonically across the expanse of a protein or molecule, resulting in Hydrogen becoming either (H1e1p) from (H2e1p)- or resulting in (H1e1p) becoming H1p without an electron.
These conditions deteriorate the neurological basis of social behavior, frontal cortex control function, behavioral conditioning, recall of conditioned stimuli/response pairs in different contexts, resiliency to externally imposed stimuli/response pairings, and include diminished Pemt ability to produce tissue plasminogen factor super clot buster, serine proteases which promote early developmental plasticity, and oxytocin which performs centrally in producing human emotional, social, group, community, civilization and species level connections and prioritization.
methylene cysteine lower than 6 um/L produces an study observed decrease from 500 instances of abated being for those with more than 6 or 7 um/L of methylene cysteine (hcy) to 1 instance of abated being among those with methylene cysteine (hcy) below 6 or 7 um/L, using two comparative populations of about 10000 participants in each group over a decade of observation.
The paradigm of programmed apoptosis and resilience are central to diminished status at physiological and behavioral levels, while also presented an important paradox between extremely resilient aging.
The mysteries continue to reveal themselves.
PEMT2 emerges at conclusion of gestation to regulated the growth and development which PEMT1 enables at conception. Mitochondria of maternal origin proliferates even before gestation while male contributed mitochondria are either inhibited or deproliferate. Mitochondria attach to numerous intracellular organelles and exchange such as endplasmic reticulum, nucleus, golgi, cytoskeleton peroxisomes, etc, to obtain Ca2+, phosphatidylethanolamine, phosphatidylserine, phosphatidylinositol and other factors, while Ca2+ is used in electron transport pathway to produce ATP, resulting in a closed loop feedback system of atp production and supply of atp from mitochondria to their interaction partners.
Pemt1 is Pemt S, short. Pemt L, for lengthened, is Pemt2 and Pemt3. The membrane shared between the endoplasmic reticulum and mitochondria is knows as the mitochondrial associated membrane. Pemt L as Pemt2 and Pemt3 are better able to traverse the increased depth or complexity, from a membrane perspective, of the mitochondrial associated membrane.
The reason that PemtL and Pemt2 in particular are pervasively diminished in disease, oncology and particularly diminished in advanced phases of conditions, is that these often involve either Impaired ability of mitochondria to import proteins, known as mPOS, or dissociation of the mitochondrial associated membrane which the literature now presents as the central loci of Pemt2 function, or both.
Improved aging involves cellular entities that behave like oncology with unusual resilience to advanced mitotic lineage including genetic, telomeric, apoptosis and mitochondrial resiliency. Oncology and disease involves similar resilience that results in paradoxes in order to achieve such resiliency.
Exhibition of senescence or differentiation to the point that cellular entities do not experience mitosis because of AP1 enabled inability of telomerase to replace telomeres, exhibition of P21, exhibition of P27 or senescent status imposed by tissue level communication such as basolateral/apical polarity.
Exracellular exosomes are used to export and import phenotype, nutrients, enzymes, metabolites, autophagic cargo, and proteins, between cellular entities in lumen or epithelium to promote uniformity. rear / front polarity is used to determine chemotaxis patterns for monocytes used for immunology or stem cellular replenish of tissue specific aggregates of stem cellular entities.
Cellular resilience and deterioration are controlled by diverse programs involving immunological, tissue level, or intracellular signaling, typically cause Bax or Bak factors promotion of apoptosis compared to Bcl2 factors counteracting apoptosis potential signaling. However, mitochondria are used in almost every pathway of programmed apoptosis or cellular level deterioration both in initiation and sustainment of signaling which results in apoptosis.
The ability of Fox proteins which enable and sustain pioneering anatomical development are now known to be result of cellular entities and stem cells to respond to the metabolic characteristics of the environment to exhibit functions of anatomical tissue inherently and aggregate and develop into such anatomical factors in layered phased development process that is less comprised of only very complicated linear development of cellular entities. This new perspective of Fox development increase the potential for pervasive regenerative outcomes including already exhibited ability to regenerate the thymus with only 1 fox protein and the ability to regenerate Islet beta cellular entities with Igf1.
PEMT inhibition results in P53 which inhibits endocytosis of glucose, inhibits entry of glucose into glycolysis, pentose phosphate and hexose monophosphate shunt pathways, causes anaerobic glycolysis, directs available pyruvate to lactate because it produces NAD+ from NADH to sustain parp signaling that can occur about 1 million times in each cellular entity each day, depletes NADH, allows parp to deplete nad+, increase Hb1ac because parp removes the ribose from NAD+ to attach it to material in promotion of a gradient upon which repair material is recruited to loci of DNA repair, and increase methylene cysteine (clinically hcy) because the nicotinamide remnants from nad+ relieved of ribose have to be detoxified by methyltransferase. Dbc1 removes its heterodimer dn from dn Dbc1 to produce Dbc1 which integrates with Sirt1 and displaces nad+ from the Sirt1 NHD nudix homology domain, resulting in Dbc1 interaction with P53 that is essential to P53 being able to convince impaired cellular entities to experience apoptosis through increases in Puma and increase in Bax. Tigar can rescue cellular entities from outcomes impose by P53, although P53 can also promote resilience. Mdm2 causes acetylation of P53 to cause it to rapidly deteriorate, although PTEN protect P53 from Mdm2.
P53 inhibits glycolysis because it is anabolic, risks genetic instability by allowing cellular entities to escape programmed apoptosis, promotes adaptation, promotes resilience, is extremely inefficient in its production of ATP compared to mitochondrial electron transport pathway and compared oxidative phosphorylation. All of these are beneficial during incipient phases of injury or impairment, while, however, promoting disease when exhibited for extended duration and without incipient phase of injury and impairment.
Aerobic glycolysis emerges when PEMT function including PEMT2 is not in place to protect a cellular entity exhibiting impaired, inadequate or nonexisting P53 function.
mPOS or isolation of mitochondria from import of proteins and dissociation of the mitochondrial associated membrane between the mitochondria and the endoplasmic reticulum, each or both results in impaired ability for decisions at the immunological, tissue and cellular level regarding resilience or apoptosis from being affected or imposed. Mitochondria can also experience resilience, and there can be hundreds of mitochondria in a cellular entity while mitochondria can move between cellular entities and exist outside of cellular entity membranes. Mitochondria dissociated from the endoplasmic reticulum or otherwise not involved in organelle exchange of Ca2+ and ATP, can import glycerol, import Ca2+ and import other metabolites directly from the cytosol and cytolplasm while causing impairment of capabilities such as exit of ribosome 80s, 60s and 40s large particles form the nucleus pore. These can cause resilient aging or resilient cellular function in impairment or injury to promote diseases.
Strategies that dissociated, reassociate, enable protein import, disable protein import, reconstitute apoptosis signaling and reconstitute resilience signaling, along with repair of mitochondrial DNA by crispr and along with repair of nucleus DNA by crispr, at some instance, possibly in the near future, are going to abrogate what is known as disease, while even now these factors may be in clinical study and development to abrogate nuances of most disease. Agrin grafts to cardiac extracellular matrix is already known to cause complete regeneration of the cardiac complex. Inhibition of Usag1 and enabling BMP7 expression are already known to cause complete regeneration of dental structures and are known to cause complete regeneration of renal structure and tissue. Inhibition of CD20 is known to stabilize even advanced renal disease. Oncology vaccines are, in some instance, having 100 percent success in producing stable and lasting remission. Populations should be acutely aware of these initiatives, fund these, move these rapidly into practice because these foundationally advance the Human experience.
The paradoxes between extreme stable homeostatic aging have emerged are possible to implement, although practice in these areas are continuing to be developed. Almost in every instance, systems’, information and information systems’ interaction with outcomes and events have caused almost every outcome or event to precise homologues to biology and have caused outcomes and events to elute precise information about the causal factors and potential resolution of pervasive aspects of diminished outcomes. Why and how outcomes occur pervasively present themselves as opportunity review, understand, counteract, prevent, learn and develop ways to improve the Human experience.
please remove all of the content submitted by the identity Researcher or similar. We are experiencing detrimental effects from the information we contributed here. The information has served its purpose, please help us reattain our health by removing the voluminous data we have contributed. We are experiencing such detriment that we must ask removal of our contributed information.
please remove the comments posted by researcher, by request of researcher. The information has served its purpose. It has caused some of us difficulty in numerous ways. Please help us be removing these comments which were meant to be helpful.
thanks
securing information flow and electron flow on web
IPv4 10.15.0.20 10.15.0.20.inaddr.arpa,
this prevents this site from being used to track and mess with contributors to the discussion
translationalwellness.com is the location of AMEHSI “A manageable and efficient health services instrumentation.” applied clinical indicators and care improvement algorithms as a system of assistive medicine, therapy, behavioral health and insight into general management of any system to more integrally, inclusively and comprehensively exhibit Human priority
Please consider the following information.
Managing methylene bridge cysteine is only 1 aspect of the foundational aspects of the systems presented here. Methylene bridge cysteine at or lower thant 6 or 7 um/L is one objective because methylene bridge cysteine deteriorates and sequesters flowing hydridic current, redox factors and the quantum energies that enable atom level structure.
The second priority is to assure available of methylene bridges that are not cysteinylated, because this enables the production of fatty acids, methyl groups, NAD, NADP, DNA RNA and foundational polymerization processes that translate current hydride, excited electrons or electrons excided from the photoelecric effect, all into structure. S-adenosylmethionine, phosphatidylethanolamine, NOPE1, NOPE2(fatty acid enabled phosphatidylethanolamine), phosphatidylcholine, DNA, omega-3 fatty acids, all are factors to use in this regard. Ethanolamine is an essential exogenously obtain nutrient as are all of the amino acids not endogenously synthesized known as the essential amino acids. Ethanolamine is recycled, but the posts or the hydrogens in CH2 methyelene bridges can wear out or structurally deteriorate like the an automobile battery, so the ethanolamine must be obtained consistently.
A typical lecithin supplement has a diverse array of phospholipids including phosphatidylethanolamine, and are good as a “daily bread” to resupply current infrastructure for efficient redox.
Finding the factors that diminish PEMT is important, that means, covering the power outlets in the home and using EMF coverings for all EMF or appliances and devices in the home. Start with covering power outlets and plugging appliances in through the tape or coverings. Obtain devices or coverings for devices and applicants to block, absorb or dissipate RF or EMF. RF and EMF are emitted by humans especially correlative to their exposure to EMF or RF, are exhibited in nature, and are exchanged by humans, devices and environmental fields, including the earth’s magnetic fields and celestial/lunar/solar sources. These are why housing and shelter, insulation, deep earth linkages to power infrastructure, all are important, although daily exposure to the earths magnetic fields at night and solar influences in the daytime, with possible participation of lunar influences, all can be essential in recycling NAD, energy infrastructure,and current. Daily sources of intended influences while also implementation of housing and shelter, all are balances derived from nature.
Also, the reason that vitamins and phytochemicare so important is that they supply current, hydride or hydridic potentiators and these fuel the carbocation activity through which molecules release fluorescent energy or 2 eV-, that enables biological activity, turns proteins into enzymes, promote alkane alkalinity that trans proteins into enzymes, and supplies energy to the environment for biological activity. A complete B vitamin with all B vitamins,B12 methylcobalamin, B6, Niacin in particular, folate, methylene tetrahydrofolate,6s 5678 tetrahydrofolate, trimethylglyine/Betaine/Beetpowder,, and/or a product such as Niagen that enables synthesis of NAD, while melatonin can help supply and recycle NAD using circadian rhythms.
The metals in vitamins also participate in magenetic interactions with systems outside of physiology to exchange current and fields in a way that enhances sustainability of redox systems.
The older one becomes, the more like that pathways that use B12 may become impaired, such that folate accumulation and B12 accumulation in circulatory fluids are linked to increasing age. The factors mentioned in the preceding paragraph open up these pathways and allow one carbon pathway metabolism to be used, such that one more pathway element becomes required.
This pathway includes going to the website where this research is presented and finding and alleviating the factors that diminish PEMT. The easiest ones are AP1 and SP! and Berberine along with Curcumin are useful, although pharmacological modulators AP1 and SP1 are available. These are strongly effective against pervasive pathology. These also inhibit NOS2 inducible.
Rubisco supplements or green leafy vegetables along with vitamin K2, can enhance hexose monophosphate shunt which reenables production of nucleotides along with availability of ethanolamine or methylene bridges.
A supplement that has diverse hexose sugars is optimal, including as a substitute for only glucose in flavorings. This is because not all hexose sugars are blocked by P53 during injury, impairment or downregulation of PEMT. Ribose is important because it supplies PARP with substrate to prevent its depletion of NAD+, Nucleotide supplements also prevent PARP from depleting NAD+. Niagen and Melatonin also enhance availability of NAD+. Availability of all the factors in the paragraph enable synthesis of nucleotides, enables parp to dissociate from the location of DNA impairment which enables optimal homologous perfect DNA repair. Also, providing these factors disables PARP as a major source of methylene bridge cysteine from nicotinamide methyltransferases as well as prevents a major foundational metabolic impairment that depletes NAD+, increases lactate anion, and deprives other pathways of pyruvate distribution from being deficient.
Once you begin focusing on alleviating the factors that downegulate methylene bridge cysteine, the faction of homocysteine produced by a functional PEMT pathways is not linked to disease.
However, it is very important to use either 33dmb, grapeseed oil, olive oil, balsamic vinegar, along with Probiotic/macrobiotic/postbiotic or broad spectrum antibiotic during an emergency to mange TMAO which is the most pervasive cause of any adverse health event or behavior.
Also mentioned should be the use of Active Hexose Correlated Compound in Latent disease vectors and other diseases because it is a choline kinase regulator and it activates the hexose monophosphate shunt bu shunting in substrates that are downregulated by P53, injury, impairment and downregulated PEMT. Regular laxatives also help clear digestive pathways of TMAO enabling factors. Bioloagically active foods, drinks, yogurts, and other capbilities have emerged in this area of therapeutics and nutrition. Although meat chicken, eggs and fish enable TMAO, there are now leaky gut supplements that are useful in this context.
Leaky gut supplements are mentioned here because sources of extracellular matrix, agrin, and laminin all enhance how these factors begin to produce regenerative effects and began regressing the effects of disease, inadequate nutrition, toxic influence or factor exposure, a detrimental factors linked with aging. Best sources of agrin include bone powder, methyl sulfonyl methane, and whole organism glandular supplement that is highly granular to prevent accumulation in digestive pathways. Agrin, laminin, whole animal glandular with leaky gut protection, methyl sulfonyl methante, enriched phosphatidylcholine, vitamin U or s methylmethionine Sulfonium, Vitamin D3 and Calcium, together make it really difficult for disease of the bone to persist while an inhibitor of NOS2 such as curcumin, ablates NOS2 as a cause of sytemic depletion of calcium and nturtients from bone. EMF protection elminates an integral cause of such conditions by preventing NOS2, phospholipase D and phosphatidylcholine specific phospholipase C.
Regardless of if you begin at the beginning, middle or conclusion of this specific list in this specific posting of information, together these provide a strong foundation for the elimination and management of any physiological or behavioral impairment. Work closely with your physician or find a health profession who most strongly believes that things happen for a reason, believes that outcomes have causality, and whom are willing to explore the causal factors of diminished and optimal outcomes, and use their knowledge, experience, wisdom, access, tools and willingness to improve human outcomes to our advantage in these contexts. There are pharmacological and therapeutics in conventional, wholistic and alternative medicine that can be applied in this regard. The objectives, pathways and strategy are most important, such that the variance in experience, perspectives and capabilities can produce even more powerfully successful outcomes in this regard.
Progress
The inherent inclination and endeavor of humanity to achieve that which circumstances do not seem to allow.
Service.
Signing off, although as we try to make this world what it can and should be, sure to encounter you all again on the road ahead.
Regards
I’ve been busy with other things and my bandwidth doesn’t currently allow me to keep up with your comments. I’ve been criticized for keeping your comments up, but I’ve found the information over the years to be intriguing. Thank you.
I am open to suggestions on how to increase my energy and capabilities, but I have developed low expectations when it comes to treating or managing myself. However some of your information has greatly helped my mother’s high homocysteine and reversed many of her conditions, so thank you for that. In particular, Enlyte has been very helpful.
Comment revised again
Importantly, it has been derived a most essential empirical observation, which is that eHcy may merely be a most obvious example of the multiplicity exhibited by methylene bridges which attach to and promote structural development and structural polymerization as well as which sequester current emitted from oxidation of Hydride or emitted current from carbocation rearrangements in molecules with hydridic character.
PEMT translates two methylene bridges protected within phosphatidylethanolamine between the Ethanolamine lead group and the oxonium exhibiting phosphate group, to exhibit only one methylene bridge while attaching three CH3 molecules to the open locations upon the ethanolamine lead group to produce choline in place of ethanolamine. The potential of methylene bridges to attach to structures and polymerize is diminished as a result and the packing of hydride into ethanolamine counteracts the methylene bridges sequestration and counteracts the susceptibility of methylene bridges to being commandeered, allowing inner membrane phosphatidylethanolamine to capture current and PEMT to package ethanolamine lead groups by packing hydride into the lead group and attach ether linked fatty enriched fatty acids to the tails as insulation.
Hcy um/L at 15 without symptoms, 19 with symptoms, otherwise above 6 9or 7, but increasing with levels further above 3.7, are thresholds for asymptomatic inpatient admittance, symptomatic inpatient admittance if not already admitted, therapeutic intervention otherwise, and focused monitoring without regard to admittance status, respectively. Hcy is a methylene bridge cysteine and when any methylene bridge molecule is not methylated or not both methylated and adenylated, or when any methylene bridge is not either stabilized or is not being deteriorated into nonmethylene bridge molecules by transsulfuration, proteolysis, autophagy, ubiquitylation, or otherwise. Ethyl molecules promote methylene bridge activity, particularly polymerization promotion, while methylation stabilizes methylene bridges.
Unmanaged methylene bridges may attach to structure, biologically active molecules, structure, promote polymerization, sequester current in these contexts, display signaling, disrupt hydridic character and carbocation rearrangements to hydridic character, and since energies are involved in structural adhesions in much if not all nuances material if the universe, the essential presumptive nuances of physics, biology and biophysics may be destabilized by accumulated, unmanaged and inadequately available methylene bridges.
Ethanolamine, de novo as nutritionally obtained ethanolamine, but recycled in pathways that can resulted in glyceryl and glucosyl phosphatidylethanolamine excluded by PEMT on its substrate selection, thus, represents this important Duality of methylene used in defense of a space in which biology may flourish along with its ability to sequester current and useful biological factors which can be overly exhibited or commandeered by less than biologically beneficial conditions.
A review of the lengthy list of required affects if Hcy or eHcy, active in or required for most if not all manifestation of diminished health status, pervasively reveal patterns of methylene bridge dysregulation, causing methylene bridge to emerge as a new most empirical specific encompassing empirical parameter in health and behavior. Particularly because methylene bridges affect the solvation shell or hydration which guides intramolecular and intermolecular interactions, as well as determines hydrodynamic characteristics at least up to 20 angstroms from the molecular surface. Methylene bridge proactive management may replace much if interventional care in developed civilizations, allowing Care infrastructure to be sustained as is with inpatient, outpatient, Office, mobile or home nuances fo care to enable vibrant industry to be sustained and grow with a correlated beneficent effect to health and behavior. This contrasts, clearly, delaying assay and care total methylene bridge mismanagement has been allowed to deteriorate physiology onto emergent or substantial pathology.
A priority is afforded to managing methylene bridges of phosphatidylethanolamine, their direction toward autophagy anchoring as glyceryl versions, their direction through exclusion from PEMT third methylation toward antihistamine function and recycling when glycosylated, as well as their preferred selection by PEMT when lightly glycosylated or unglycosylated. Ethanolamine attaches the fatty acids to ctp – ethanolamine using diacylglycerol or allocated acylglycerol as linkages while this catalytic interaction prefers sn-1,2 diradylglycerol as substrate, result in in major output as phosphatidylethanolamine and some fraction glycerophosphatidylchol7ine. Oxidative phosphorylation, cellular respiration Complex III enabling, essential phosphatidylserine decarboxylase translation of phosphatidylserine to phosphatidylethanolamine occurs at the inner mitochondrial membrane such that sn-1,2 diacylglycerol phosphatidylserine and sn-1,2 diacylglycerol are Selectively preferred as substrate by both phosphatidylserine decarboxylase 1 and phosphatidylserine decarboxylase 2.
These conclusions present how interconnected systems and incentives that promote information sharing and divulgence of information, may be among the most powerful developments among the Universes, particularly if excluding the first instance in which organisms exhibited the inclination to benegicently care for one another. Such inclination, in objective opinion, changed everything that has since emerged and has changed everything that may ever be.
Revised comment
For your information, it has been derived he strongest empirical observation, which is that eHcy s merely an most obvious example of the multiplicity exhibited by methylene bridges which attach to and promote structural development and structural polymerization as well as which sequester current emitted from oxidation of Hydride or emitted current from carbocation rearrangements in molecules with hydridic character.
PEMT translates two methylene bridges protected within phosphatidylethanolamine between the Ethanolamine lead group and the oxonium exhibiting phosphate group, to exhibit only one methylene bridge while attaching three CH3 molecules to the open locations upon the ethanolamine lead group to produce choline in place of ethanolamine. The potential of methylene bridges to attach to structures and polymerize is diminished as a result and the packing of hydride into ethanolamine counteracts the methylene bridges sequestration and counteracts the susceptibility of methylene bridges to being commandeered, allowing inner membrane phosphatidylethanolamine to capture current and PEMT to package ethanolamine lead groups by packing hydride into the lead group and attach ether linked fatty enriched fatty acids to the tails as insulation.
Hcy um/L at 15 without symptoms, 19 with symptoms, otherwise above 6 9or 7, but increasing with levels further above 3.7, are thresholds for asymptomatic inpatient admittance, symptomatic inpatient admittance if not already admitted, therapeutic intervention otherwise, and focused monitoring without regard to admittance status, respectively. Hcy is a methylene bridge cysteine and when any methylene bridge molecule is not methylated or not both methylated and adenylated, or when any methylene bridge is not either stabilized or is not being deteriorated into nonmethylene bridge molecules by transsulfuration, proteolysis, autophagy, ubiquitylation, or otherwise. Ethyl molecules promote methylene bridge activity, particularly polymerization promotion, while methylation stabilizes methylene bridges.
Unmanaged methylene bridges may attach to structure, biologically active molecules, structure, promote polymerization, sequester current in these contexts, display signaling, disrupt hydridic character and carbocation rearrangements to hydridic character, and since energies are involved in structural adhesions in much if not all nuances material if the universe, the essential presumptive nuances of physics, biology and biophysics may be destabilized by accumulated, unmanaged and inadequately available methylene bridges.
Ethanolamine, de novo as nutritionally obtained ethanolamine, but recycled in pathways that can resulted in glyceryl and glucosyl phosphatidylethanolamine excluded by PEMT on its substrate selection, thus, represents this important Duality of methylene used in defense of a space in which biology may flourish along with its ability to sequester current and useful biological factors which can be overly exhibited or commandeered by less than biologically beneficial conditions.
A review of the lengthy list of required affects if Hcy or eHcy, active in or required for most if not all manifestation of diminished health status, pervasively reveal patterns of methylene bridge dysregulation, causing methylene bridge to emerge as a new most empirical specific encompassing empirical parameter in health and behavior. Particularly because methylene bridges affect the solvation shell or hydration which guides intramolecular and intermolecular interactions, as well as determines hydrodynamic characteristics at least up to 20 angstroms from the molecular surface. Methylene bridge proactive management may replace much if interventional care in developed civilizations, allowing Care infrastructure to be sustained as is with inpatient, outpatient, Office, mobile or home nuances fo care to enable vibrant industry to be sustained and grow with a correlated beneficent effect to health and behavior. This contrasts, clearly, delaying assay and care total methylene bridge mismanagement has been allowed to deteriorate physiology onto emergent or substantial pathology.
These conclusions present how interconnected systems and incentives that promote information sharing and divulgence of information, may be among the most powerful developments among the Universes, particularly if excluding the first instance in which organisms exhibited the inclination to benegicently care for one another. Such inclination, in objective opinion, changed everything that has since emerged and has changed everything that may ever be.
For your information, it has been derived he strongest emperical observation, which is that eHcy s merely an most obvious example of the multiplicity exhibited by methylene bridges which attach to and promote structural development and structural polymerization as well ascwhich sequester current emitted from oxidation of Hydride or emitted current from carbocation rearrangements in molecules with hydridic character.
PEMT translates two methylene bridges protected within phosphatidylethanolamine between the Ethanolamine lead group and the pxonium exhibiting phosphate group, to exhibit only one merhylene bridge while attaching three CH3 molecules to the open locations upon the ethanolamone lead group to produce choline in place of Ethanaolamine. The potential of methylene bridges to attach to structures and polymerize is diminished as a result and the packing of hydride into ethanalomine counteracts the methylene bridges sequestration and counteracts the susceptibility of methylene bridges to being commandeered, allowing inner membrane phospatidyl ethanolamine to capture current and PEMT to package ethanolamine lead groups by packing hydride into the lead gouo and attach ether linked fatty enriched fatty acids to the tails as nsulation..
Hcy um/L at 15 without symptoms, 19 with symptoms, otherwise above 6 9or 7, but increasing with levels further above 3.7, are thresholds for asymptomatic inpatient admittance, symptomatic inpatient admittance if not already exhibited, therapeutic intervention, and focused monitoring, respectively. Hcy is a methylene bridge cysteine and when any methykene bridge molecule is not methylated or not not both mefhylated and adenylated, or when any methylene bridge is not being deteriorated into nonmethylene bridge molecules by trasukfurration, proteolysys, autophagy, ubiquitylation, or otherwise.
Unmanaged methykene bridges may attach to structure, biologically active molecules, structure, promote polymerization, sequester current in these contexts, display signaling, disrupt hydridic character and carbocatio rearrangemts to hydridic character, and since energies are involved in structural adhesions in much if not all nuances material if the universe, the essential presumptive nuances of physics, biology and biophysics may be destabilized by accumulated, unmanaged and inadequately available methylene bridges.
Ethaolamine, de novo as nutritionally obtained ethanolamine, but recycled in pathways that can resulted in glyceryl and gluosyl phosphatidylethanolamine excluded by PEMT on its substrate selection, thus, represents this important Duality of mthykene used in defense of a space in which biology may flourish along with its ability to sequester current and useful biological factors which can be overly exhibited or commandeered by less than biologically beneficial conditions.
A review of the lengthy list of required affects if Hcy or eHcy, active in or renquired for most if not all manifestation of diminished health status, pervasively reveal pattrrs of methylene bridge dysregulation, causing methylene bridgeto emerge as a new most emperical magic or emerical managemnt parameter in health and behavior. Methylene bridge proactive management may replace much if interventional care in developed civilizations, allowing Care infrastructure to be sustained as is with inpatient, outpatient, Office, mobile or home nuances fo care to enable vibrant industry to be sustained and grow with a correlated beneficent effect to health and behavior. This contrasts, clearly, delaying assay and care total methylene bridge mis Management has been allowed to deteriorate physiology onto emergent or substantial pathology.
These conclusions present how interconnected systems and incentives that promote information sharing and divulgence of information, may be among the most powerful developments among the Universes, particularly if excluding the first instance in which organisms exhibited the inclination to benegicently care for one another. Such inclination, in objective opinion, changed everything that has since emerged and has changed everything that may ever be.
Our computing devices have been commandeered and impaired. The work we have done on the sitrs and on the software has paused because if these. People assisting in development are being shunned and ostracized for working on these important priorities. This is why our internet links are not active, because we cannot even sustain ourselves to do the free work.
Work will continue once we have or funding or when people performing free work no longer are being shunned from obtaining work otherwise.
Estmated, about 10,000 people everyday in on Nation alone, and many more orally may be incurring detrimental outcomes and abating being unnecessarily because our participants are being ostracized, denied work, or because funding has not been allocated to these efforts.
Regards and continue access the content for trandlationalwellness and amehsi research. We are your advocates, although work has now paused because our workers are being prevented from working to sustain themselves and this prevents even free work on these important issues from occurring.
It’s our opinion that people should be allowed to sustain themselves even while the devote their free time to assurance of vital being.
jalajava2@gmail.com
Hi,
Connected with ‘a researcher’ several years ago on this site, on the topic of choline deficiency, and received guidance at the time. Is this still the same correspondent? Can’t locate ‘amehsi’ online anymore.
Thanks,
RV
10, 8. Roger that. look for translationalwellness website. removed some the foundational and controversial research because of the potential for it being commandeered for misinformation. Only the essential artifacts and derivitizations are on the site now. However, much of these derivitization analysis are presented in these discussions. The data in these discussions and at translationalwellness website, should help anyone and health services provider or group of providers, practitioners and clinical case managers as well as civilization level services workers to prevent, intervene and alleviate almost any dimiinished outcome include disease, adverse health events, behavioral health conditions, chronic conditions, and adverse behavioral outcomes. Once we find a way to present the foundational research in a way that prevents is misuse, we may reintegrate these in a foundation research area within the translationalwellness site.
good to know you are here, potentially benefiting from information here, and continuing to contribute. Its been a long road, but this information is now emerging and advancing toward assure human therapeutic and behavioral outcomes.
it is important to observe that the information provided here is not intended to impugn an service, systems, group, industry or individual. The way that groups and those llinked to one another in different ways have been required to peruse linkages of causality, events, contexts, and pathways in order to fully apply knowledge and capabilities to their benefit, is merely presented here. Groups supporting their members and those with home they are associated can become focused on producing inefficient supporting mechanisms, resulting in omitting of emerging coverages, funding, assistance and services that have occurred. Particular referential context and experience are presented here by searchers and users, and these are not intended to be critical of any systemic actors because those actors have endeavored upon the path of service, and hardly anyone places themselves through the ordeal education, training and service to assure that optimal outcomes do not occur, but typically do so in the endeavor of improving Human outcomes. Amazingly supportive aspects of care coverage, health service coverage, care, occupational and other therapy, all have emerged in an increasingly humanist way. The interactions produced and presented here by most, including this researcher merely impugn diminished Human outcomes themselves because the empirical nuances of reason seem to strongly suggest that Humans are intended to only incur favor, particularly in how humans interact with one another.
Caregivers, providers and individuals require assistance early in their lives and early pathology as well as until reconstituted function occurs. These include planning that only includes optimal outcomes. The massively improved nuances of health services provision and health services assurance should be commended on such improvement, although these endeavors may have continued path of improvement to achieve the favor which has been intended for Humanity.
Also, please look beyond the spelling and grammatical errors because of the massive amounts of information and translative activity that was required and the priority of getting information out for analyses and implementation.
Regards
A summarization of therapeutic recommendations for Viral conditions, including clearance of viral pathogens linked to disease, as well as pathologies ubiquitously is presented, again.
These factors may comprise ubiquitously effective solution, although nearly existing 130 factors are outstanding. These factors are relevant for minor conditions, allergies, chronic conditions, impairment, autism, detrimental behavior. psychiatric conditions, pyschological conditions, genetic conditions, complications, risk for perioperative complications, etc.
Add these factors in order, observing the affect of each additional factor. HPV, HIV, most any viral condition, oncology, and pervasive disease are relevant to this info.
This information is relevant to prevent and reverse the adverse effects of aging. It is also relevant for regeneration of anatomy including reconstituted impaired neurological, muscular and other function, including congenital disease. This information is also relevant for myasthenic conditions including parkinson’s disease, etc.
Avoid Milk and dairy unless its made from or constituted of A2 Milk.
Avoid meat, chicken, eggs and fish unless its micronized and probiotics and prebiotics are utilized with these.
Probiotic, Prebiotic, Postbiotic and live, living foods.
Focus on nonGMO organic foods.
Every night before sleep, a prebiotic, Grapeseed Oil, extra virgin fruity polyphenol enriched olive oil or Balsamic Vinegar.
Curcumin or an SP1 inhibitor.
Berberine or an AP1 inhibitor.
Active Hexose Correlate Compound AHCC or an inhibitor of Choline Kinase alpha.
Active Hexose Correlated Compound AHCC or an inhibitor of iNOS inducible Nitric oxide Synthase.
Danshen, Red Sage or Salvia M in pill or tablet versions.
S-methylmethionine Sulfonium or a product known as Gastromend HP.
Methylsulfonylmethane or MSM.
A complete B vitamin with B12 Methylcobolamin included.
Trimethylglycine or N,N,N Glycine Betaine.
The product EnlyteRX.
L-arginine.
Tetrahydrobiopterin.
6s 5678 Tetrahydrofolate.
It also becomes essential to supply foundational aspects of cellular function, lipids and cholesterol not made or produce in a laboratory.
A mixture of grapeseed oil, extra virgin fruity olive oil, blackseed oil, mixed together along with sesame seed oil if the sesame seed oil does not cause allergies. Several ounces in the morning and several ounces in the evening.
It may help to cover the electricity plugins or outlets in dwellings with duct tape or inflammation resistent Tape.
Using Faraday enclosures or EMF covering for electronic devices, appliances, as bedding and sleepwear can be helpful.
An air purifier also can assist in lower levels of systemic inflammation.
To counteract aging or extend this list as necessary.
Pregnenolone counteract diminished star protein provision of shielded transfer for cholesterol to the mitochondria.
Phosphatidylserine complex from vitamin shoppe(phosphatidylethanolamine, phosphatidylserine, phosphatidylcholine, phosphatidylinositol).
Phosphatidylcholine at least 400 mg.
Dr Scheussler’s Salts all 12 combined.
Whole animal glandular/matrix supplement.
Bone Powder Supplement.
Agrin Supplement, Graft or Injection, although agrin promotes regeneration along with interleukin 11, such that the signaling invoked by Agrin can enhance cellular proliferation requiring that it be omitted if oncology exists. However, matrix deterioration, scaring and stiffness as well as inadequate obtainment of lipids and cholesterol not made in a laboratory are major foundational conditions for disease and oncology because these cause persistent inflammatory signaling and involve al aspects of physiology. Mini Agrin is better along with apoptosis inhibiting drugs or apoptosis inhibition generally to enable regeneration of neurological, muscular, pathways, function, including congenital conditions.
Matrix Electrolyte Powder.
These may be helpful without utilizing the list to analyze all of the indicators with regard to the condition or circumstance an individual may have. Although, using the list oneself and with a clinician is best because this allows a professional who is focused on managing, understanding and monitoring these to work for you in an efficient manner.
Eradicating HIV and other latent viral factors.
These suggest that Istodax, Ingenol Mebutate, Panobinostat and Bryostatin, together may have broad enough coverage to cause HIV latency clearance.
HDAC Inhibitors and Histone Methylation Inhibitors may be effective.
However, stabilization of stabilization of the G4 quadruplex using TMPyP4, BRACO-19 and TRIM22 along with these may be especially effective.
Protein Kinase C inhibitors generally may by effective.
Inhibitors of SP1 may be particularly useful, including TRIM22 but also including pharmacological inhibitors as well as curcumin or berberine.
Ingenol Mebutate along with JQ1 latency reversal factor that is small molecular bromodomain inhibitor.
The utilization of CRISPR Genome editing capabilities to eliminate viral and latent viral affliction, as well as repair genetic disease and alleviate accumulated genetic impairment, particularly when utilized with transduction domains that enable therapeutics to permeate all cellular types with the efficiency of a water molecule, may be indispensable in this regard and there should be galvanization of populations to have such therapies rapidly developed.
General Viral Affliction linked to disease. RNA polymerase inhibition.
Artichoke, Favipiravir, or Cidofovir or other.
Information. Ebiomedicine. Volume 63. Number 103159. 2021. PMID 33340992.
EGFR, GSK3alpha, ARIH1 comprise a pathway to deteriorate PDL1 to enhance resilience to oncology by allowing cellular entities exhibiting oncology to be found more adequately. However, if there is any manner of immunological dysfunction or inhibition, this mechanism can be less than adequately effective. EGFR is also known as HER1. ARIH1, however, inhibits hnRNP E1 which represses pathogenic, oncology promoting and mesenchymal transition enabling mRNA elongation and translation. hnRNP E1 is also inhibited by Homocysteine.
EGFR is upregulated in oncology of the reproductive organs including cervical, breast, prostate and other oncology. hnRNP E1 inhibition by any means is known to enable viral conditions to escape into pathology including HPV, HIV, PV(myelitis).
Inhibiting EGFR, GSK3 alpha or ARIH1, or inhibiting Homocysteine, in reproductive tissues can alleviated oncology reliant upon EGFR. Oncology that relies upon GSK3 are diverse and more numerous than those of reproductive tissues. Oncology reliant upon homocysteine are somewhat inclusive of all oncology. However, the now exhibition of these factors for diverse and expansive groups of viral disease and oncology linked to viral disease are pivotal.
Importantly, the analyses produced thus far, after perusing these pathways and interactions, concludes that SP1 inhibition may disable this nexus of disease somewhat completely, preventing even signals from the pituitary that promotes SP1 as well as signals from physiology and the environment from commandeering these pathways for pathogenic potential. SP1 was indicatively involved and essential to these pathway’s sustained exhibition.
SP1 inhibitors can be obtained as pharmacological factors or include curcumin, turmeric, irinotecan and other factors.
Curcumin inhibits GSK3B. EGFR is inhibited by curcumin or genistein. There are numerous pharmacological inhibitors of EGFR and GSK3B. Homocysteine management is presented on and in the translationalwellness website. Inhibition capabilities for ARIH1 are to be included when they are incurred, but are likely to already be in development, testing and approval, although natural therapies are likely to already exist.
Typically, a mechanistic link that is direct that explains homocysteine enablement of disease is elusive, often requiring systematic changes and cellular survival changes to be explained. However, HPV is enabled to escape from repression by hnRNP E1 because homocysteinylation of hnRNP E1 impairs the ability of hnRNP E1 to inhibit or impede the transcription of oncological and pathogenic migration transition enabling mRNA into long coding mRNA that is used for synthesis of proteins that enhance oncology pathogenesis as well as enable oncology migration. hnRNP E1 integrates into Cysteine dense regions of the 3’UTR of mRNAs in correlation to TGFbeta availability.
hnRNP E1 is relevant for HPV, HIV, and PV(myelitis).
hnRNP E1 is also downregulated by the ubiquitinase ARIH1, and experimentally inhibition of hnRNP E1 by ARIH1 results in mesenchymal transitions as well as enhanced pathology in breast tissues affected by oncology. Inhibition of the Ubuitinase ARIH1 can delay oncology pathology and prevent mesenchymal transitions. ARIH1 protects cellular entities from exhibition of toxicity enabled impairment of the genome. ARIH1 signaling causes PDL1 to become deteriorated. A study observes that ARIH1 overexpression can produce therapeutic apoptosis in neoplasms, except when immunocomprimised statuses are exhibited, presumably because deterioration of PDL1 prevents obscuring of cellular entities exhibiting oncology such that removing the obscuring influence of PDL1 requires immunological competent signaling to result in apoptosis. The EGFR/GSK3alpha/ARIH1 signaling pathway produces ubiquitylation of PDL1.
However, experimental expression of of pathways that invoked EGFR performed when EGFR has been prevented from being expressed, result in exhibition of the dehydrogenase DPD that deteriorates the therapeutic 5FU as well as invoked expression of the familiar factor SP1. EGF, the growth factor linked to the EGFR receptor, could be instrumented to cause upregulation of SP1 expression and upregulation of DPD, although both gefitinib and mithramycin A suppressed both SP1 and DPD confirming the known role of mithramycin A in suppressing SP1. Information. BMC Oncology. Volume 16. Number 354. 6th Month, 2016. PMCID PMC4896005. Information. Mol Cellular Biol. Volume 35. Number 7. Pages 1254 to 1268. April 2015. PMID 25624349. Journal ISSN Number 14765594. “ARIH1” 2022. Information. PMID 31681852. PMCID PMC6824538. Information. The Journal of Nutrition. Volume 147. Issue 4. April 2017. Pages 471 to 472. March, 2017.
EGFR and Activin A overexpression in oral squamous carcinoma were inhibited by inhibition of INHBA which is subunit of activin and inhibin as well as which inhibits secretion of FHS follicle stimulating hormone or gonadotropin or glycoprotein polypeptide hormone from the anterior pituitary gland gonadotropic cellular entities. FSH is known to modulate development, maturation growth as well as changes to reproductive tissues along with reproductive processes in physiology. Inhibition of INHBA downregulated EGFR, inhibited Activate A ability to produce canonical Smads which are small molecule signal transducers that affect transforming growth factor beta and TGFbeta’s ability to modulate or regulate cellular development and cellular growth. INHBA inhibition also prevented phosphorylation of AKT at serine 473, rephosphorylation of phosphorylated AKT at serine 473 and phosphorylation of SP1. Information. Sci Rep. Volume 9. Number 1. Pages 5197. March, 2019. PMID 30914776.
This same study observed that SP1, SP1 coactivator crotonylation writer P300 as CBP/p300, as well as Smad protein, all were recruited to the EGFR promoter after Activin A instrumentation. These clearly present that SP1 canonical crotonylation activity and promoter activity causes or enhances expression of EGFR and this activation of EGFR by SP1 can be the result of multiple influences, stimuli or circumstances that mimic Activin A stimulation resultant of inhibition of INHBA which is an original, anatomical signaling molecule produced from the anterior pituitary. SP1 signaling can be commandeered by pathogenic factors, influence or circumstance to mimic original signaling derived from the pituitary. Although INHBA inhibition enabled Activin A expression in this study, it is important to know the INHBA is a subunit of Activin, INHBA suppresses Activin A such that anterior pituitary activity can inhibit SP1 through inhibiting Activin A, suggesting release of SP1 for catalysis occurs when this anterior pituitary signaling is inhibited or diminished because of pituitary dysfunction or deterioration.
Inhibition of PI3K resulted in inhibited SP1 activity, such that PIRK activity upregulates both AKT phosphorylation at Serine 473 and SP1. This presents a mechanism by which conditions in the physiology environment can commandeer signaling pathways controlled or induced by the anterior pituitary.
Luteinizing hormone as well as human chorionic gonadotropin hCG integrate into the luteinizing hormone/chorionic gonadotropin receptor LHCGR to maintain corpus luteum function. hCG and presumably luteinizing hormone activity the LHCGR while experimentation suggests that FSH does not. Importantly, hCG was experimentally able to activity steroidogenesis hormones. Both activation of LHCGR and activation of steroidogenesis were prevented by inhibition of SP1. Human primary luteinized granulosa cellular entities are able to be expressed resultant of activation activity in the proximal region of the LHCGR. SP1 and GATA5, as complex, may be involved in maintaining of adequate LHCGR Expression. Information. J Steroid Mol Biol. Volume 190. Pages 183 to 192. 6th month, 2019. PMID 30954507.
Inhibiting SP1 may be an alterative to intricate and invasive therapy that requires analysis and phenotype diagnostics because it can disable the EGFR expression system in EGFR linked oncology.
GSK3alpha and GSK3B are considered to be affected by the same inhibitor patterns. GSK3B can be inhibited by curcumin or turmeric.
Indirubin, Tideglusib, Indirubin 3’ Oxime, Alterpaullone, Resibufogenin, 5 Bromoindole, 1 Slskrnpsullonr, BIO, Bikinin, Bio Acetoxime, BRD0705, 9 ing 41m and MAZ51 are inhibitors of GSK3, GSK3alpha and GSK3beta. Information. GSK3. The Selleckchem.com website.
Ubiquitylation includes a proteasomal system and can function even when selective autophagy is not available.
However, ARIH1 upregulation also produces inhibition of hnRNP E1. Homocysteine can inhibit hnRNP E1 as well.
EGFR is upregulated in oncology of the cervix and oncology of the breast, including enabling escape of HIV, HPV and PV(myelitis) from protective effects of hnRNP E1 on pathogenic mRNA elongation and translation.
Upregulated EGFR, upregulated GSK3B, upregulated ARIH1 and Homocysteine all may be therapeutically inhibited to improve outcomes in oncology of breast and oncology of cervix, including HPV enabled oncology as well as HIV, and PV(Myelitis).
EFGR and HER1 are refer to the same status or protein. Curcumin or turmeric, Genestein, both inhibit EGFR and HER1.
Olertinib, Osimertinib, neratinib, gefitinib, cetuximab, dacomitinib, panitumumab, lapatinib, necitumumab, mobocertinib, and vandetanib are all inhibitors of EGFR approved by the FDA for utilization.
Afatonib or gilotrif ss approved for EGFR genetic polymorphism L861Q, S7681 and G719X. Afatonib is approved for NSCLC oncology specifically, but is an EGFR inhibitor. Afatonib is also approved for EGFR genetic polymorphism comprised of exon 19 substitutions and exon 21 L858R substitutions, as well as for mesenchymal transition characterized, squamous, NSCLC oncology in which therapy with platinum enabled chemotherapy becomes ineffective.
Information. Oncology Letters. Volume 22. Issue 3. Published Article Number 646. September, 2021. July, 2021.
Information. “Natural Products that Inhibit.” Curr Oncol. Volume 13. Number 3. Pages 99 to 107. 6th Month, 2006. PMC1891180
FSH alpha subunit is expressed on cytogenic location of 6q14.3 in basophils of the anterior pituitary. The beta subunit is expressed at 11p13 in gonadotropes of the pituitary cellular entities. FSH components are transactivated in response to Activin as well as inhibited by inhibin. FSH signaling stimulates expression and determines level of EGFR synthesis.
Removal of reproductive tissue, ovariectomy, resulted in upregulation of alpha subunits and beta subunits among inhibin which exhibits two beta subunits for inhibin as a homodimeric factor as well as among activin B which exhibits an alpha subunit for Activin and a beta subunit for activin, as well as upregulated Follistatin. Each of these, activin B, inhibin B and Follistatin are regulators of FSH. Experimental administration of GnRH in pituitary tissue incipiently produced incipient downregulation of the alpha subunit of activin B, downregulation of beta subunits of both Activin B and Inhibin B, followed by a secondary phase after extended duration of 20 hours that resulted increases in 100 nM of GnRH that increased expression of these subunits.
Experimental instrumentation of GnRH produced an incipient upregulation of Follistatin. Extended duration exhibition of Estradiol and inhibin B inhibited expression of the beta subunit, while this extended duration had no determinable affect on alpha subunits and Follistatin. This explains why the analysis of Inhibin elsewhere in this document observes inhibin B subunits as an inhibitor of Inhibin.
The expression of inhibin, activin, as subunits, and expression of Follistatin, each expect gonadal or reproductive tissues as feedback inhibitors, presumably to establish developmental homeostasis. Ovariectomy diminishes such feedback and results in unregulated alpha, beta subunits and unregulated Follistatin. Estradiol is particularly expressed in reproductive tissues and causes even activation of Estrogen Receptor Alpha and Estrogen Receptor Beta, while these two receptors regulate one another as well as Beta activation of AP1 and Alpha inhibition of AP1 which is important because AP1 inhibits activation of PEMT also. This is important because this oscillating mechanism produced by estradiol in reproductive tissue exhibiting increased levels of estradiol mimics the activity of inhibin B in repressing activity by beta subunits which are essential for inhibin catalytic activity. Reproductive tissue, Estradiol and Inhibin B autoregulate GnRH levels in the pituitary, while reproductive tissue deterioration, removal or impairment can cause increased levels of GnRH, increasing FSH production, and in this context FSH is an upregulator or stimulator of EGFR. However, in optimal contexts and typical conditions, the feedback mechanisms of reproductive tissue must be inhibited or diverted to enable upregulated expression of EGFR.
Estrone, derived from fat, estradiol or testosterone, causes overactivation of estrogen receptor alpha compared to lowered expression of estrogen receptor beta. Diminished estradiol, preventing even activation of estrogen receptors is linked to impaired estrogen levels, impaired testosterone level, deterioration of physiology, susceptibility to disease, menopauses, increasing levels of homocysteine, and susceptibility of estrangement of the mitochondria from the endoplasmic reticulum including isolation of PEMT2, obliteration of PEMT2, and essential components to all manifested disease.
Beta subunits of inhibin, or inhibin has to be suppressed or inhibited, or activin A has to be substantially upregulated compared to inhibin, or estradiol must be downregulated, in the context of reproductive tissue, in order for FSH to produce upregulation of EGFR. These provide an intricate linkage between the function PEMT, the differences of estrone/estradiol/estetrol/estriol in reproductive compared to nonreproductive tissues, as well as establish the feedback mechanisms by which these interact in typical, impaired or therapeutically changed metabolism.
Information. Proc Natl Acad Sci U S A. Volume 111. Number 47. Pages 16778 to 16783. November 25, 2014. Information. J Endocrinol. Volume 210. Number 1. Page 71 to 79. July, 2011. PMID 21490134.
Activin A and Activin B are in the group of TGF beta factors. Thus, Activation of Activin A and Activin B performs activation of PI3K and Smad Pathways that compete for shared consensus sequences within the SP1 integration loci generally, but particularly occurring in the EGFR proximal promoter. Prevailing of Smad in this competition results in SP1 EGFR activity that involves crotonylation, while prevailing of PI3K results in EGFR expression. Experimental inhibition of INHIBIN A in oral oncology resulted in repression of EGFR, repression of Activin A Smad activation, downregulation of phosphorylated AKT at serine 473, and downregulation of AKT phosphorylated at Serine 473, as well as repression of SP1. This confirms that Inhibin inhibits Activin A.
EGFR2, HER2 or ERGG2, in contract to other EGFR versions that variably integrate with ligands in the extracellular exposed aspects of the transmembrane protein which can be as many as 11 extents of extracellular exposed protein, does not integrate with any ligands, having particular nuance of pathology. This explains why HER1 and HER2 are distinctively represented in the literature. The extracellular domains can be activated by ligands to produce autophosphorylation of tyrosine kinases in the intracellular environment, activating PI3K/AKT, Ras/MEK/ERK, PLCy/PKC which activates protein kinase C and catabolism of phosphatidylcholine specifically from cellular membranes requiring more activity by PEMT and CDP Choline Pathways, JAK/STAT, all of which are linked to pathways of survival, inflammation, cellular proliferation described in this document in numerous instances, including mesenchymal transitions.
Although PEMT2 ablation has about 100 percent of oncology, including oncology of the breast, EGFR upregulation is found in between 30 and 15 percent of oncology of breast, while perusing the axis to include homocysteine, hnRNP E1 inhibition, viral or other disease, GSK3B upregulation and ARIH1 upregulation, as well as SP1 upregulation, can be pervasively linked to oncology while in reproductive tissues, these factors can be linked to expansive if not all disease. This is because genetic anomaly in these pathways and invoking of other translational wellness indicators can often involve invoking of SP1. SP1 seems to be invoked as protective mechanisms, as might many of the indicators in such regard, when compared to AP1, but can be commandeered by pathology, pathogens or circumstance. Downregulation of BRCA1 and upregulation of tissue transglutaminase both can upregulate EGFR metabolically, although other analyses here, at the translational wellness site, and among the no longer publicly published translational wellness information, clearly observe numerous PI3K, mitogenic, developmental and other signaling that upregulate SP1, Smad, TGFb group of actors, etc. These include environmental factors. Regardless of how naturopathic therapies make sense and might be preferred, nutraceutical and pharmacological capabilities may be essential in counteracting what may be pharmaceutical levels of influence produced by the environment. Importantly, pharmaceuticals may have to utilize pathways different from the cytochrome p450 pathways now utilize, by using cleaner, greener and more specifically and tangentially active factors.
Information. “Role of HER2, EGFR, and other Receptor Tyrosine Kinases in Oncology.” Oncology Migration Rev. Volume 35. Number 4. Pages 575 to 588. December 2016. PMCID PMC5215954.
Information to Include in the therapeutic list. A
Eradicating HIV and other latent viral factors.
These suggest that Istodax, Ingenol Mebutate, Panobinostat and Bryostatin, together may have broad enough coverage to cause HIV latency clearance.
HDAC Inhibitors and Histone Methylation Inhibitors may be effective.
However, stabilization of stabilization of the G4 quadruplex using TMPyP4, BRACO-19 and TRIM22 along with these may be especially effective.
Protein Kinase C inhibitors generally may by effective.
Inhibitors of SP1 may be particularly useful, including TRIM22 but also including pharmacological inhibitors as well as curcumin or berberine.
The utilization of CRISPR Genome editing capabilities to eliminate viral and latent viral affliction, as well as repair genetic disease and alleviate accumulated genetic impairment, particularly when utilized with transduction domains that enable therapeutics to permeate all cellular types with the efficiency of a water molecule, may be indispensable in this regard and there should be galvanization of populations to have such therapies rapidly developed.
Viral Specific Factors that destabilize Replication, Transactivating Protein Phosphorylation and SP1, including three levels of HIV function.
Durhamycin, Mithramycine and Chromomycin, add a multiple level therapeutic that can added to more completely abrogate diverse aspects of HIV and other viral pathology.
Hormone Linked Therapy in Oncology and Viral Conditions.
Upregulated EGFR, upregulated GSK3B, upregulated ARIH1 and Homocysteine all may be therapeutically inhibited to improve outcomes in oncology of breast and oncology of cervix, including HPV enabled oncology as well as HIV, and PV(Myelitis). It is very likely that much more expansive oncology and viral conditions are therapeutically affected by managing these factors. Certainly, this explains gender differences in outcomes with viral conditions. Inhibitors of hnRNP E1 otherwise may also be inhibited as required specifically in oncology of reproductive tissues. Importantly, inhibition of SP1 disables much of this system at multiple levels for use therapeutically in oncology or reproductive issues.
However, the literature observes that steroidogenesis or hormone synthesis as well as steroidogenic Cytochrome P450 genetic transcription relies upon SP1 in some way. Analysis revealed that although two SP1 integration loci as well as 3 Steroidogenic Factor 1 integration loci are exhibited in the StAR protein promoter region in genome. Cytochrome P450 versions are ubiquitously utilized in pharmacotherapeutic processing, such that SP1, like most factors observed in the list of translaitonalwellness factors, produce a more empirical affect that escapes complexities exhibited in cytochrome p450 systems of processing, although disabling of this complexity may change or affect how drugs, pharmacological factors, therapies impose change in physiology. One benefit is that pharmacotherapeutic usage of cytochrome P450 pathways can compete with PEMT for methyl group resources resultant COMT processes and prodrug activation processes.
SP1 has been found to be utilized when PI3K, cAMP signaling and Pituitary INHBN enablement of Activin, all perform activation of hormonal functions, such as upregulation of EGFR, activation of steroidogenic cytochrome P450 proteins and transactivation of StAR proteins that enable shield transport of cholesterol across diverse membranes into the inner mitochondria where Cytochrome P450 produces pregnenolone, the incipient factor in steroidogenic pathways as well as the original potent inhibitor of choline kinase for selective production of enriched phosphatidylcholine by PEMT. However, a study observes that SP1 integrates with SF1 and this complex attaches itself to the SF1 promoter and to the two SP1 promoters that are near SF1 integration loci within promoter regions.
Disabling SP1 can have a massive inhibiting effect to hormonal activity and probably should be utilized carefully if used for anything but limited duration. EGFR inhibitors, GSK3B or GSK3A inhibitors, ARIH1 inhibition and Homocysteine inhibition may be powerful in managing oncology of reproductive tissues. Information. Endocrinology. Volume 141. Number 8. Pages 2895 to 2903. 9th Month, 2000. ARIHI1 and Homocysteine inhibit hnRNP E1 which is an escape mechanisms for disease, viral vectors, and oncology, such that managing GSK3B, EGFR, EGFR2, ARIH1 can be therapeutic if oncology exists or a viral condition exists, particularly if these are affecting reproductive tissues.
Reproductive tissue produce Estradiol until deterioration occurs such as menopause, aging or other disease, and estradiol represses activin A similarly to repression of activin A/B by inhibin beta subunits. This repression activity is negative feedback regulator that decreases expression of GnRH and thereby decreases FSH. FSH stimulates Activin A which then performs as a TGFb factor to enable expression of Smad, PI3K, phosphorylation of AKT at Serine 473 and competitive interactions among these to assist SP1 integration into the EGFR promoter. However, FSH activation of Activin A requires repression of the inhibin beta subunit because this subunit inhibits activin A/B.
Reproductive tissue produces Estradiol in greater amounts than other tissue such that deterioration of reproductive tissue, disease, menopause, aging and diminished PEMT function, as well as repressed steroidogenesis, results decreased exhibition of negative feedback to FSH production by the anterior Pituitary. Removal of reproductive tissue can also produce upregulated FSH. This enables upregulation of EGFR suggesting that inhibin beta subunits expect reproductive tissues to provide a negative feedback influence to manage EGFR levels.
Estrogen receptor alpha and beta both cause transcription of PEMT. Importantly, Estradiol is important because it evenly activates estrogen receptor alpha and estrogen receptor beta such that beta version regulates alpha version, also such that alpha version and beta version oppositely regulate AP1, and AP1 is an inhibitor of PEMT activity. Uneven overactivation of Estrogen Receptor Alpha results in diminished PEMT activity and overactivation and dysregulation of steroidogenic signaling, glucocorticosteroid signaling, and diminished PEMT catalytic activity.
SP1, is involved in environmentally activated, toxicity activated, viral activated, canonical and other pathway activation of this complete program. Inhibiting PEMT destabilizes disease that emerges in this pathway, but also should be considered for limited duration. Extended duration inhibition of these hormonal pathways can result in upregulation of the inhibited hormones and this biphasic phenomenon explains why ubiquitously effective estrogen inhibition therapy, before exhibition of more diverse therapy in the existing era, resulting in a typical reemergence of disease after about 1 or 2 years. Estradiol is typically a more powerful and health promoting metabolite compared to estrone, particularly because estrone can be derived from fatty tissue without a metabolic priority for doing so.
The factors utilized to eradicate HIV should include these.
Ingenol Mebutate along with JQ1 latency reversal factor that is small molecular bromodomain inhibitor.
Information. Ebiomedicine. Volume 63. Number 103159. 2021. PMID 33340992.
The mysteries keep unfolding. Eradicating HIV and other latent viral and latent microbial conditions.
Analysis reveals that SP1 is the factor that determines HIV switch from lytic status to latency. This suggest that G4 quadruplexes may exhibit SP1 in numerous or voluminous instances, and latency of viral vectors may pervasively involve either SP1, G4 quadruplex, or other transcriptional factors in G4 Quadruplexes that commandeer L – Arginine and produce this, what might be described as canonical model of latency used by microbes or viruses. Most importantly, it is known that AP1 inhibition clears some diseases caused by HPV, and enhances or enables clearance of HPV viral vectors, such as in Berberine’s ability clear HPV.
The literature observes that histone deacetylase and histone methyltransferase inhibitors result in activation of latent HIV which confirms the observation that SP1 is displaced from promoters in the Glutathione transcriptional region in two places by methylation of SP1 integration loci, such that inhibition of methylation upon histones specifically would increase availability for methylation of genome otherwise, presuming conditions of increased methylation generally. Similarly, SP1 promotes acetylation of genome, particularly by recruiting P300 to loci of DNA impairment to perform NHEJ nonhomologous repair and P300 is a histone deacetylase that also acetylates P53 to enhance its duration before ubiquitylation or proteolysis. Information. DNA Repair. Volume 105. Article 103171. 2021.
These present that histone acetylase inhibitors and histone methylation inhibitors counteract SP1. These are known strategies for HIV eradication in the literature. Moreover, the literature observes that removal of histone lysine crotonylation Kcr reactivates latent HIV, such that P300 performance as crotonylation factor is diminished by inhibition of SP1, preventing SP1 recruitment of P300 to the genome. ACSS2 is known to provide crotonylation CoA to those crotonylation factors at the HIV LTR to enable post translational modification through crotonylation by crotonylation writers such as P300.
NFkB has been presented in the literature as an activator macrophages, neutrophils, interferon and pathways linked to these, protecting from the affects of viruses, bacteria and pathogens. Canonical NFkB signaling and activation produces ubiquitinated NEMO/ATM that is able to return to the cytosol to phosphorylate IKKB which then activates noncanonical NFkB by phosphorylating the IkB component of NFkB, causing deterioration of IkB. Simultaneously, RelA/P50 complexes experience translocation to the nucleus where it begins gene transactivation. Canonical NFkB is causally linked to transcriptions in which IkB alpha deterioration enables canonical NFkB signaling cascade that results in translocation of p65/P50 into the nucleus. However, inhibition of or low expression of canonical NFkB, as well as impaired translocation of canonical NFkB to the nucleus is linked to latency. Inhibition of IkB in these contexts results in reactivation of HIV, enabling HIV to exit from latency.
Protein Kinase C agonists can mimic diacylglycerol isoforms and integrates into the regulatory domains of PKC isoforms, changing the PKC/canonical NFkB pathway in a way that causes IkB to become deteriorated, activating HIV from its latent status. Ingenol mebutate PEP005, ingenol B, phorbol esters such PMA/TPA, Prostratin, bryostatin-1, other agonists of PKC. Among these prostratin analogs, Bryologs or Bryostatin1 analogs, Ingenol Mebutate along with JQ1 latency reversal factor that is small molecular bromodomain inhibitor, but particular the latter of these, results in reactivation of latent HIV at high volume levels, even with only 1 treatment or instrumentation.
The FDA approved drug PICATO clears conditions linked to advanced HIV and among older members of HIV affected populations, although PICATO is a topical gel that implements Ingenol Mebutate. Observation of instrument observed no adverse affects other mild inflammation at location of topical instrumentation while systematically PICATO resolve clinically obvious systems, decreased indicators of paused or latent stages of HIV in both CD4+ and skin cellular biopsies, did not exhibit obvious reactivation or enhanced inflammation of the immunological system, all which are indicators of systematic reactivation of latent HIV, which is interesting because the study participates continued to be on Antiviral therapies to repress HIV replication. This contracts with typical toxicity of Protein Kinase C inhibitors which is so typical that hydrid nanocarriers have been synthesized for Ingenol mebutate to enhance efficacy in latency reversal as well as diminish potential for adverse effects.
Euphorbia Kansui, EK, is rife with Ingenol derivatives, and is being tested as a tea to be ingested therapeutically to reactive latent HIV.
HDAC inhibitors and Ingenol Mebutate are effective in activating latent HIV. HDAC inhibitors alone were limited in their effect. Ingenol was inclusive able to induce HIV exit from latency in all tested tissue and cellular entities. Bryostatin1 exhibited targeted latency activation in particular cellular versions. Istodax and Ingenol Mebutate increased HIV RNA among most tissues and cellular types, Panobinostat with Byostatin1 had the ability to upregulate HIV RNA in memory stem cellular entities.
These suggest that Istodax, Ingenol Mebutate, Panobinostat and Bryostatin, together may have broad enough coverage to cause HIV latency clearance.
However, stabilization of stabilization of the G4 quadruplex using TMPyP4, BRACO-19 and TRIM22 along with these may be especially effective.
Protein Kinase C inhibitors generally may by effective.
Inhibitors of SP1 may be particularly useful, including TRIM22 but also including pharmacological inhibitors as well as curcumin or berberine.
The utilization of CRISPR Genome editing capabilities to eliminate viral and latent viral affliction, as well as repair genetic disease and alleviate accumulated genetic impairment, particularly when utilized with transduction domains that enable therapeutics to permeate all cellular types with the efficiency of a water molecule, may be indispensable in this regard and there should be galvanization of populations to have such therapies rapidly developed.
Information. Ebiomedicine. Volume 63. Number 103159. 2021. PMID 33340992.
Sorting through the mystery of health, important observations emerge. Disease and impairment can be assisted by immunological, xenobiotic and other function. SP1 is invoked in pervasive disease and can be inhibited by particular contexts, resulting in complexity that is difficult to understand unless the complete list of translationalwellness indicators are analyzed. SP1, for instance, is upregulated and causes latency of HIV and other viral conditions mostly through inhibition of transcription that makes viral conditions difficult to ascertain by immunological factors. Similarly, SP1 upregulates PD1 and PDL1 which obscures cellular entities from lymphocyte monitoring. Importantly, the effect of electromagnetic and wireless fields can become obscured or diminished by particular response mechanisms. SP1, for instance, enables expression of OGG1 which protects neurons from electromagnetic energy exposure, such that inhibition of SP1 leads to expanding levels of DNA impairment in neurons.
These interactions can be numerous, and does not indicate that wireless and electromagnetic energy are not detrimental because increasing levels of homocysteine and levels inflammation can cause changes and escaping of particular mechanisms, resulting in wireless and electromagnetic energy being either cumulative or emerging as very detrimental in particular contexts. Similarly genetic conditions, genetic change, nutrition, therapeutics or other factors can change SP1 or other factors individually, resulting in an escape mechanism for disease.
These are interesting because the infrastructure rebuilding legislation that was presented in the year preceding this one, should have included complete insulation, encapsulation and mitigation of electromagnetic energy from powerlines, infrastructure, dwellings, transformers, power generation stations, as well as assuring communications wiring and infrastructure are likewise insulated. This would lower the baseline levels of homocysteine in the population and result in a remarkable increase in average span of vital being and decrease both detrimental behavior and disease, as well as level of impairment among populations. Although more innovative changes to wireless communications are required to diminish the influence of these to populations, such as ascertaining harmonious frequencies, utilize wired connection points when possible, or other changes, diminishing the influence of electromagnetic fields from electricity infrastructure is likely to cause about a decade or more difference in average span of vital being. Similarly, though, the 2009 changes to wireless communications resultant of the 2005 communications act, and imposition of cable transmittal of communications, was counteracted by movement of many communications vectors to wireless and mobile devices. Thus, at least after insulating, repairing, enclosing all communications pathways and electricity infrastructure that is wired, there may be adequate focus on how to make wireless communications more and more safe for populations.
securing information flow and electron flow on web
IPv4 10.15.0.20 10.15.0.20.inaddr.arpa,
this prevents this site from being used to track and mess with contributors to the discussion
an island in the central Pacific Ocean
These factors may comprise ubiquitously effective solution, although nearly existing 130 factors are outstanding. These factors are relevant for minor conditions, allergies, chronic conditions, impairment, autism, detrimental behavior. psychiatric conditions, pyschological conditions, genetic conditions, complications, risk for perioperative complications, etc.
Add these factors in order, observing the affect of each additional factor. HPV, HIV, most any viral condition, oncology, and pervasive disease are relevant to this info.
This information is relevant to prevent and reverse the adverse effects of aging. It is also relevant for regeneration of anatomy including reconstituted impaired neurological, muscular and other function, including congenital disease. This information is also relevant for myasthenic conditions including parkinson’s disease, etc.
Avoid Milk and dairy unless its made from or constituted of A2 Milk.
Avoid meat, chicken, eggs and fish unless its micronized and probiotics and prebiotics are utilized with these.
Probiotic, Prebiotic, Postbiotic and live, living foods.
Focus on nonGMO organic foods.
Every night before sleep, a prebiotic, Grapeseed Oil, extra virgin fruity polyphenol enriched olive oil or Balsamic Vinegar.
Curcumin or an SP1 inhibitor.
Berberine or an AP1 inhibitor.
Active Hexose Correlate Compound AHCC or an inhibitor of Choline Kinase alpha.
Active Hexose Correlated Compound AHCC or an inhibitor of iNOS inducible Nitric oxide Synthase.
Danshen, Red Sage or Salvia M in pill or tablet versions.
S-methylmethionine Sulfonium or a product known as Gastromend HP.
Methylsulfonylmethane or MSM.
A complete B vitamin with B12 Methylcobolamin included.
Trimethylglycine or N,N,N Glycine Betaine.
The product EnlyteRX.
L-arginine.
Tetrahydrobiopterin.
6s 5678 Tetrahydrofolate.
It also becomes essential to supply foundational aspects of cellular function, lipids and cholesterol not made or produce in a laboratory.
A mixture of grapeseed oil, extra virgin fruity olive oil, blackseed oil, mixed together along with sesame seed oil if the sesame seed oil does not cause allergies. Several ounces in the morning and several ounces in the evening.
It may help to cover the electricity plugins or outlets in dwellings with duct tape or inflammationproof Tape.
Using Faraday enclosures or EMF covering for electronic devices, appliances, as bedding and sleepwear can be helpful.
An air purifier also can assist in lower levels of systemic inflammation.
To counteract aging or extend this list as necessary.
Pregnenolone counteract diminished star protein provision of shielded transfer for cholesterol to the mitochondria.
Phosphatidylserine complex from vitamin shoppe(phosphatidylethanolamine, phosphatidylserine, phosphatidylcholine, phosphatidylinositol).
Phosphatidylcholine at least 400 mg.
Dr Scheussler’s Salts all 12 combined.
Whole animal glandular/matrix supplement.
Bone Powder Supplement.
Agrin Supplement, Graft or Injection, although agrin promotes regeneration along with interleukin 11, such that the signaling invoked by Agrin can enhance cellular proliferation requiring that it be omitted if oncology exists. However, matrix deterioration, scaring and stiffness as well as inadequate obtainment of lipids and cholesterol not made in a laboratory are major foundational conditions for disease and oncology because these cause persistent inflammatory signaling and involve al aspects of physiology. Mini Agrin is better along with apoptosis inhibiting drugs or apoptosis inhibition generally to enable regeneration of neurological, muscular, pathways, function, including congenital conditions.
Matrix Electrolyte Powder.
These may be helpful without utilizing the list to analyze all of the indicators with regard to the condition or circumstance an individual may have. Although, using the list oneself and with a clinician is best because this allows a professional who is focused on managing, understanding and monitoring these to work for you in an efficient manner.
Reverse osmosis incorporating activated carbon and activated carbon filtration can remove PFO, Teflon, phthalate, C8 particulate from water. Information. PFOA and PFOS. Msterwaterwater.com Master Water Conditioning Company Website. High pressure filtration system membranes or filters can remove PFOAS. Information. Crit Rev Environ Sci Technol. Volume 49. Number 24. Pages 2359 to 2396. 6th Month, 2019. PMID 32831535. There is voluminous literature on the correlated effects of PFOAs to development from embryonic to to adult phases. The literature has established levels at which development of emerging mammalian physiology can be ablated by PFOAs exposure, although generally, PFOAs contributed to, enhance or more rapidly enable exhibition of pathophysiological conditions including affecting prognosis, levels of disease or phases of disease. Information. PMID 35022659. Diverse emerging mechanisms of managing PFOAs include Source management, deterioration, bioremediation, electrocoagulation, Foam fractionation, photocatalysis, use of sound, mechanochemical, electrochemical, electron beams, and plasma.
PFOA exposure promotes enhanced pathogenic activity in oncology of tissue of the breast. PFOA exposure increased cyclin D1, increased CDK4/6 as well as produce a decrease in P27, although PPAR alpha antagonism diminished this pathological enhancement, suggesting that PFOA involves homocysteine, upregulation of choline kinase and fatty acid metabolism changes. Information. Ach Toxicol. Volume 92. Number 5. Pages 1729 to 1739. 2018. PMID 29502166. Estrogen Receptor inhibition did not alleviate exposure to PFOAs in this study, explaining a source of oncology that is resistant to estrogen therapy. Gastrodin attenuates PFOA enabled hepatic injury, through regulation of digestive pathway microbiota in small nonhuman mammals. This suggests that PFOAs may seep into physiology through impaired digestive membranes when exhibited in food, water, and environment. Information. Bioengineered. Volume 12. Number 2. Pages 11546 to 11556. 2021. PMID 34866532. Gastrodin improves peripheral neuropathy linked to oncology therapy, particularly in oncology of breast tissues.
Similarly, Gastrodin produces enhanced immune response in oncology therapy and prevents hepatic ascitic neoplasm growth using upregulation of CD4+ Lymphocyte NFkB to enhance immunological activity. Although plantamajoside herbal supplement and Betulinic Acid were specifically found to be effective in breast oncology therapy, Gastrodin improve peripheral neuropathy and hepatic oncology parameters, experimentally in context of PFOA, phthalate, C8 or teflon exposure. The literature links PFAS, Teflon and some other ‘forever chemicals’ with oncology of the reproductive tissue and splanchnic organs in particular. These analyses link every version of oncology except particular oncology resultant of increased levels of trimethylaminenoxide with upregulated homocysteine. The data clearly supports these correlations, while the data also demonstrates clearly that PFOAs upregulated homocysteine. PFOA levels, thus can be correlated to every disease that relies upon upregulated homocysteine, which is, every disease and pervasive detrimental behavior and behavioral health conditions.
Gastrodin is among the known, experimentally analyzed, modalities of decreasing PFOAs, although managing homocysteine can diminish the detrimental effects of PFOAS. Isoliensinine, Kurarinol each were affective in producing apoptosis in hepatic oncology. Information. “Perfluorooctanoic Acid (PFOA), Teflon, and ‘linked’ Chemicals.” Information. Medicine. Volume 99. Issue 27. Page e20936. July, 2020. Information. Drug and Chemical Toxicology. 2018. Pages 1 to 8. PMID 30554535. Information. Toxicology and Applied Pharmacology. “Betulinic Acid.” Volume 275. Number 2. 2014. Information. Bangladesh Journal of Pharmacology. Volume 8. Number 4. Pages 414 to 419. December, 2013. Lobetyolin inhibits breast oncology by inhibiting ASCT2, presumably through sensitivity of proteolytic upregulation in oncology exhibiting cellular entities to depletion of nutrients that ASCT2 provides, such as cysteine, alanine, and serine. The conclusion however, is that PFOAs can be environmental, in food, from cooking using teflon, in water, or from particular household factors. Reducing these can assist in managing homocysteine and molecular influences in oncology. Information. Human and Experimental Toxicology. Volume 40. Issue 12. Pages 2074 to 2086. 6th Month, 2021. PFOA activates ppar alpha, diminishes ppar gama, inhibits HNF4 alpha, and transcriptionally upregulates Cjn/Cfs transcription factors which are abbreviated in this paragraph, but doe not result in phosphorylation of these two factors, which are essential, when phosphorylated for AP1 transcription. Human duration of exhibition for PFOA and PFOS which are no longer allowed to be distributed or utilized in products, is about half of a decade.
PFOA exposure cause experimental transition of typical breast epithelial cellular entities to exhibit migration, distal integration, and infiltration activity, as well as neoplastic transition and as well as proliferation. P27 and P21 were diminished by PFOA/PFOS and P53 was upregulated, while cyclin D1 phosphorylation at threonine 286 was diminished, and ERK1/2 phosphorylation were increased. P38 was either upregulated or upregulated in phosphorylated fraction by PFOA/PFOS. Acetylation of H3K9 were inhibited while dimethylated H3K9 was decreased in PFOA exposed cellular entities. These do not include all PFOA/PFOS but present how these factors change factors that determine status and outcomes in oncology, particularly oncology of breast tissues. Information. Arch Toxicol. Volume 94. Number 11. Pages 3893 to 3906. July, 2022. PMID 32700164. Information. Toxicology. Volume 333. Pages 53 to 62. July 3, 20215. PMID 25868421.
Another study found that AP1 was enhanced by PFOA while estrogen receptor alpha was inhibited which could be caused by AP1 inhibition of Estrogen Receptor Catalysis, although pregnane X receptor was upregulated which is context of xenobiotic and endobiotic transport systems utilized in pharmacological and prodrug metabolisms such as cytochrome p450 versions 3x and 2x. Although constitutive androstan receptor was upregulated by PFOA, HNF4 alpha was inhibited. This study, from the information accessible, did not present phosphorylation of AP1 as a result of PFOA exposure. Information. “PFOA.” The Institute for Risk Assessment. 2013.
PFOA was found to cause increase, correlative to PFOA levels, in methylation of the SP1 integration loci in the Glutathione S transferase Pi promoter region. This methylation might displace SP1. However, PFOA is known to decrease histone H3K14 of the StAR promoter resulting impaired development and reproductive function. PFOA also inhibits Estrogen transcription through StAR promoter repression and through Estrogen Receptor Alpha inhibition, resulting in diminished synthesis of oxytocin receptor linked to PEMT enabled Oxytocin signaling. Oxytocin is an essential factor in human emotional linkages and stability, such that this context may present a promoting of these factors from molecular, to physiological, behavioral and social levels. Information. Endocrinology. Volume 147. Pages 899 with 13 pages of content. Information. Toxicol Sci. Volume 148. Pages 368 to 379. Information. Toxicology. Volume 333. Pages 53 to 62. July 3, 2015. PMID 25868421.
Another study observes that GSTP exhibits 2 SP1 integration loci and methylation of these prevents the ability of SP1 to counteract AP1 transcriptional upregulation. Importantly, because P21 and P27 are diminished by PFOA, PFOS, these suggest another correlation between SP1 activation and exhibition of P21 and P27 cellular cycle pause junctures. Information. International Journal of Chemotherapy Research and Practice. Volume 1. Number 1. Page 4 to 30. 2018.
The information presented here was probably more complex than necessary, although an ancillary objective was to provide enough detail to enable a clinician to review what a patient or other individual might have encountered within the information presented.
$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$
“Clearly, management or inhibition of homocysteine, s adenosyl homocysteine, AP1, SP1, iNOS, uncouple NOS and Cholilne Kinase, using Active Hexose Correlated Compound as well as therapeutics, supplements, neutraceuticals or other mechanisms of managing these may eradicate HPV, destabilize or eradicate HIV, may be prevent or eradicate pervasive other viral conditions, parasites fungal conditions, microbial or bacterial affliction, an expansive group of oncology versions that even includes voluminous oncology conditions that are not linked to microbial affliction.” This list, although possibly nearly 100 percent effective is likely to change since the review is only at indicator list item 4 or 130 and only has analyzed subset of linked conditions and has only analyzed a focused set of the data and literature for each condition. Stay tuned.
$$$$$$$$$$$$$$$$$$$$$$$$$$$$$
Importantly, do get better information, review the translationalwellness.com site because in the next few paragraphs, a simplistic group of things to do will be presented that will be qualified with some, interesting and to many readers possibly difficult to believe information. Only a small amount this controversial but true information will be presented here to qualify the recommendations.
Right now, during the development of level 5 artifacts at translationalwellness.com, the 130 or more indicators or causal factors of disease and detrimental outcomes have been correlated to their relevance in disease and link to factors that inhibit as well as upregulated or modulate each indicator in the list present as level 1 and level 2 indicator list artifacts. Level 5 presents this same list of 130 factors in tabular structure as elements of a column or list, while diseases, toxins and detrimental outcomes are listed in the columns adjacent to the list. Interestingly, at this juncture only 4 clinical indicators have analyzed in the context of 3 conditions or disease, but because of the remarkable results, many similar disease and diverse other disease were rapidly reference cursorily to see how expansive these none other than pivotal results for the first few indicators really may be.
HPV was used as one of the first group of factors reviewed because it is so intricately and comprehensive characterized in the literature and data. HIV was included because it exhibits an insight laden paradox that is relevant to pervasive viral conditions and disease. The other factors included in the first group of analysis were selected and will be selected in a manner that exhibits homologous contexts and divergence nuances that lead the way to understand large aspects of the conditions and outcomes exhibited among populations. No clear plan to produce a taxonomy from such linkages, homologues and divergence, although this might emerge as an essential capability.
Regards.
The analysis clearly demonstrates the fourth factor, pretty much every disease falls apart and becomes simply explainable using a canonical module of PEMT inhibition, mitochondrial seperation from the endoplasmic reticulum, Parp signaling, transcription cascade by AP1, transcriptional silencing to produce latent disease by SP1, upregulation PD1/PDL1 by SP1 to cause disease cellular entities to hide from immunological monocytes, along with homocysteine upregulation apoptosis and a response to this by upregulation of survival pathways that become oncology because this survival response becomes persistent due to SP1 enable latency and SP1 enabled hiding of disease cellular entities. Choline kinase upregulation which is required in all disease as well as iNOS upregulation and uncoupling were added, although the analysis of each disease has not reach that row in the list of inidcators, because active hexose correlated compound has emerged as an iNOS inhibitor and an inhibitor of choline kinase.
Clinicalfactor Disease/toxicfactor/outcome1 Disease/toxicfactor/outcome2 ” ” ”
1.Clinicalfactor HIV HPV
2 Homocysteine hcy 1 (essential and causal) 1 (essential and causal )
3 s adenosyl hcy 1 1
4 AP1 1 1
5 SP1 1 (latency factor) 1 (latency factor)
6 (outoforder, iNOS) 1 1
7(ooouncoupled iNOS) 2(causal, latency correlated) 2 (causal and latency correlated)
6 and 7 were added because active hexose correlated compound modulates these.
Remarkably, when we applied these mechanisms in cursory review of diverse viral disease, even the bacteria analyzed, and parasites reviewed, as well as disease such influenza, general oncology, etc, the disease fell apart like a house of cards, almost suggesting that the disease should no longer exist or should not have existed, particular in the modern era.
HIV, for instance, was analyzed in the context of TB. Instrumentation of Active Hexose Compound occurred at 3 g for about 6 months, although another study is in place now that reviews 6 g per day dosages. The study did not intend to therapeutically affect HIV but improve TB outcomes and therapeutics toxicity.
All clinical symptoms among the HIV/TB group were improved by month 3. There were 0 patients among 35 with cough or hemoptysis. 100 percent of AHCC receiving patients had improvement in breathing depth impairment. 100 percent of AHCC receiving patients had complete recovery of impaired appetite. 96 percent of patients had recovered lost anatomical mass that was diminished during the course of the disease. Nausea was completed abrogated from the group of patients receiving AHCC. Regurgitation was completely abrogated in the group receiving AHCC. Pulmonary structural assay using visualization diagnostics revealed that although improvement occurred in both placebo and AHCC receiving groups, 92 percent of the AHCC group had recovered to typical pulmonary structural characteristics.
Information. “AHCC.” Teikyo Medical Journal. Volume 44. Issue Number 3.
It is important to know that lists or stacks of versions of viral, oncology, impairment, disease, genetic disorders and other factors, voluminous lists, are presented in the literature as being benefited or abrogated, as well as having abrogated symptoms from these factors.
These include conditions such as Parkinson’s disease also. Again, the analysis is only at item 4 or item 6 or 7 of 130. The analysis has briefly endeavored to go wide in ascertaining the breadth of these 6 or 7 factors to understand if the list can really be 10 instead of 130. Although each such analysis potentially reveals that another underconsidered factor should be promoted to be among the list of detrimental factors.
The manner of clinical study, clinical work, and therapeutic analysis, as well as care required to produce such studies and information is remarkable and a credit to those able to produce such arduous analysis, tasks, and outcomes information
Importantly, there are pervasive homologous to this data in human outcomes and outcomes among systems, even those outcomes which are considered to be detrimental and including those outcomes which are considered to be optimal. Although vital being and optimal human outcomes however possible, not merely however practical, should and are always system priorities, these demonstrate that systems may often be analyzed or scrutinized according some of the somewhat impossible assure practical objectives or popular ideas of utility for such systems. These analyses suggest that true objective of systems may be to work together to produce the observations, information, and understanding that allows analysis, critical thinking, discoveries and ways of improving human outcomes to occur. These big objectives in which humanity moves forward toward transcendence seem to be obscured by the focusing events that occur at geopolitical, political, national, regional or other levels. Such that humanity might improve the condition of humans and the effectiveness of systems in assuring Human outcomes, there must be a status quo from which such improvement or transcendence might occur.
Clearly, management or inhibition of homocysteine, s adenosyl homocysteine, AP1, SP1, iNOS, uncouple NOS and Cholilne Kinase, using Active Hexose Correlated Compound as well as therapeutics, supplements, neutraceuticals or other mechanisms of managing these may eradicate HPV, destabilize or eradicate HIV, may be prevent or eradicate pervasive other viral conditions, parasites fungal conditions, microbial or bacterial affliction, an expansive group of oncology versions that even includes voluminous oncology conditions that are not linked to microbial affliction.
securing information flow and electron flow on web
IPv4 10.15.0.20 10.15.0.20.inaddr.arpa,
this prevents this site from being used to track and mess with contributors to the discussion
Mysteries Do Unfold.
Canonical Exhibition of Viral and Oncological Latency, and confirmation of the essential, required, preventable, causal, treatable, and mappable causes of disease at the cellular level. The lenses of CRISPR and the ability to edit out genetic disease, viral genome inserted into genome, and microbial genomes themselves to deactivate pathogens, opens the possibility of closer analysis of industry knowledge no longer required for industries to produce therapeutics. Revealing the mechanisms of disease and demonstrating the pervasive disease have been able to be cured for decades. Unshared secrets, information and knowledge, transformed the centuries which have come before the existing era. The new generation of Industry members have opened the commodities of the generations for review and supplanting these with truly transcendent therapeutics.
Guanine dense regions of DNA have the propensity fold or loop, and these loops or folds can occur in multiplicity within the same sequence of nucleic acids or among different sequences of nucleic acids, such as that these may the stack upon one another in tetrads or quadruplexes. Guanine enhanced nucleic acids sequences can occur in RNA and DNA, as well as can produces within the primary and secondary, as well as tertiary structure, but may also occur through quaternary structure that emerges in 3D association of these folds or loops in the way that DNA relaxed or condensed in its helical structure or resultant of histone packing and unpacking. G4 or G quadruplexes can exhibit genetic sequences which perform as ligands. Transcriptional factors can be located in these folds, such as SP1 and NFkB, often being linked to changes in transcription.
The canonical model of Hominid G4 G quadruplexes number near 100,000 in the genome and occur within the telomere regions that must be between 10 and 50 TTAGGG repeats which characterize telomere regions. The literature clearly links choline and folate, or methyl group deficiency, with telomere attrition and as a primary pathway of chromosome fusion that stably deactivates genome replication and solve the telomere maintenance paradox but produces cellular senescence or exist from replication with substantial impairment of responsiveness to environmental change.
G4 or G quadruplexes, thus, require stable telomeric function. G4 Quadruplexes are stabilized by molecular stabilizers and interestingly by Cations such as Potassium or K+ which nestles into the groove between the quadruplexed folds similar to where the Hoogsteen Hydrogen linkages that characterize atypical interstrand linkages between leading strand and lagging strand in the Watson Crick Groove especially when G4 or G quadruplexes are exhibited. Pyridostatin, 4,5 Dimethoxy 2 nitrobenzyl bromide, PhenDC3, TMPyP4 are four factors that are known to stabilize G4 quadruplexes. These factors variably modulate G4 G quadruplexes. Information. Search for Pyridostatin at Sigmaaldrich.com.
Microbial G4 Quadruplexes, however, benefit microbial, viral, fungal, parasite or other pathogen persistence, replicative variability, transcription, and virulence, among other ways of enhancing pathogen activity.
G4 G Quadruplexes require, or occur, typically within or near 10 or 50 TTAGGG sequences or telomeres. SP1 and AP1 oppositely regulated hTERT or human telomere reverse transcriptase which adds Telomere sequences to DNA once they have been decreased by multiple instances of DNA replication occurring in particular cellular circumstances such as meiosis or mitosis. SP1 is mentioned in some contexts along with the TATA box structure that imposes regulation and control of transcription processes, although SP1 can occur in many genes and is known to occur in all hominids. HPV, however, exhibits repression of particular protein synthesis by SP1 which presents in an interesting paradox, because SP1 is a ubiquitous factor in viral activity. However, complete analysis of the literature reveals that SP1 is an enabler of other phases of HPV pathology and is a repressor not in atypical sense, but causes decisions to be made about which version of HPV and what modality of pathologies might emerge.
A review of the literature clearly presents that AP1 inhibition cause clearance of some viral vectors including some HPV but widely represses HPV replication. SP1 is widely causal or active in latent viral status such as in HIV, EBV, HSV and numerous pathogenic viral vectors including EVD/EHF. The specific factor causing latency is sometimes debated, but the mechanisms offered for latency typically omit precise mechanisms. The known utilization of methyltransferases to obscure viral DNA used by Viruses presents how methylation obscures viral DNA but do not describe how a cellular entity is caused to persist along with latten or hidden microbes within such cellular entity. This context is revealed by the activities of G4 quadruplexes, particularly, SP1 exhibited in G4 quadruplexes. A Study of catalytic cascade engineering utilized G4 quadruplexes to produce citrulline from L-arginine, suggesting that iNOS in HIV virulence, although pervasive other viruses utilize iNOS, exhibits lytic viral activity and replication using iNOS, while when iNOS becomes uncoupled, HIV becomes latent. The continued activation of G4 complexes, thus, produces a cyclic deprivation of L – Arginine from HIV in a way that produces a switch from lytic to latent status, while the directing of L – Arginine to citrulline promotes macrophage polarization to inflammatory M1 phenotype that is sustained somewhat stably and continuously by G4 quadruplex production of citrulline from L -arginine particularly because citrulline is efficiently translated into L – Arginine.
However, the characteristics of latency in this context are none other than pivotal. The G4 Quadruplex depletion of L -Arginine leaves HIV or other viral vectors available to deplete Ca2+ and the depletion of Ca2+ is not, according to the literature a feature of iNOS uncoupling, such that L – arginine depletion is the primary cause of iNOS uncoupling. The depletion of Ca2+ causes the mitochondrial associated membrane which is comprised of cooperative, communicative and transport proteins to deteriorate resulting in estrangement of the mitochondria from the Endoplasmic reticulum. These produce an impaired ability for Mitochondria to activate, promote and assure completion of apoptosis pathways that are used to deteriorate diseases cellular entities and are highly conversed immunological function in complex organisms. Similarly, the dissociation of the mitochondria from the endoplasmic reticulum not only produces inability to prevent latency, but constitutes latency, as well as results in inability of phosphatidylserine and phosphatidylethanolamine, and phosphatidylinositol and Ca2+ to be provided to the mitochondria from the endoplasmic reticulum. These cause the decrease in catalysis, diminished productivity and then, eventual, obliteration of PEMT2 that characterizes, canonically, oncology in pervasive versions.
Analysis reveals that SP1 is the factor that determines HIV switch from lytic status to latency. This suggest that G4 quadruplexes may exhibit SP1 in numerous or voluminous instances, and latency of viral vectors may pervasively involve either SP1, G4 quadruplex, or other transcriptional factors in G4 Quadruplexes that commandeer L – Arginine and produce this, what might be described as canonical model of latency used by microbes or viruses. Most importantly, it is known that AP1 inhibition clears some diseases caused by HPV, and enhances or enables clearance of HPV viral vectors, such as in Berberine’s ability clear HPV.
However, pivotally, Active Hexose Correlated Compound has demonstrated clear 40% effectiveness with 1 g and 60% effectiveness with 3 g ability to clear HPV that has already become oncology of cervical tissues. These suggest that increased dosages might be able to achieve 100 percent or extended duration of any such dosage might be linked to near 100 percent effectiveness in eliminated oncology and other disease produced by HPV as well as eliminating HPV affliction. Information. JPEN, J Parenter Enteral Nutr. Volume 31. Number 5. Pages 373 to 380. September and October, 2007.
Most pivotally, when the mechanisms of action were analyzed for Active Hexose Correlated Compound, this mechanism included management of MAPK linked pathways. However, when iNOS was searched for along with Active Hexose Correlated Compound, the literature irrefutably presented that Active Hexose Correlation Compound inhibits iNOS or inhibits inducible nitric oxide synthase.
Also, an analysis of the research presents that Active Hexose Correlated Compound exhibits Adenosine and Adenosine is a known downregulator of Choline Kinase Alpha, NFkB, Interleukin Type I receptor, Choline kinase alpha upregulation is not only essential but is pervasively required in oncology and is pervasively required in disease that have a cellular pathology compound. It is not clear which, if any, diseases do not have a cellular pathology component. Information. PloS One. Volume 12. Number 8. e0182775. Information. Nitric Oxide. Volume 40. Pages 75 to 86. 8th Month, 2014. PMID 24878381.
Choline Kinase has been known of since at least the 1950s and 1960s, with Purinyl – L – Histamine being known as a choline kinase inhibitor, such that it is not clear why therapeutics have not been developed, produced and become stabilized in care and in the industry, particularly since histamine therapy in oncology has been known of since 1910s. However, because dimethylthetin has been known to manage homocysteine since 1878, there is nothing remarkable about such an omitted beneficial factor since the most beneficial factors seem to also haven been omitted. These analyses expect or present a strong possibility that even more remarkable capabilities that have been known, produced, been possible, or might be readily available as the level 5 translational artifact becomes produced. Certainly, CRISPR capability to edit disease out of the genome including pathogenic insertion of genetic material, as well as including editing out a pathogen’s enabling genetic sequences within the pathogen itself, all are producing a context in which knowledge, and industry, may be finally transcending the current set of physiological mechanisms. These may be why the omitted capabilities are moving from trade or industry secrets into the light of human observation and translation into utility as well as understanding that can be integrated into care processes or therapies rapidly. Certainly, the current industry and the humans in the relevant industries are likely to have been essential in allowing such information to move into plain human observation.
Berberine, Active Hexose Correlated Compound, and many of the other factors presented here such as turmeric/curcumin, specifically inhibiting SP1, AP1 and iNOS, may be pervasively destabilizing to disease, oncology., viral disease including HPV, HIV, EVD/EHF, the disease enabling the pandemic of 2020 to 2021, HSV, EBV, particularly viral vectors somewhat comprehensively. Mot pivotally, the literature clearly presents that studies of G4 modulation have resulted in elimination or eradication of latent HIV when coupled with other transcription inhibitors to manage lytic HIV along with G4 quadruplex modulation to eliminate latent HIV. Information. Molecular Oncology. Volume 10. Article 39. 2011. PMID21496227. Information. National Library of Medicine Clinical Study Number NCT04633330. Information. Front. Oncol. Volume 9. Page 173. 2019. PMID 30949451.
HPV16 E6 upregulates SP1 and hTERT Increasingly with duration of exhibition of HPV but, again, SP1 can be upregulated in diverse phases and nuances of viral activity, particularly when involving DNA and RNA transcription, replication, cellular entry, persistence, latency and other ways. Information. PloS One. Volume 12. Number 8. Article e0182775. 8th Month, 2017.
HPV E2 transcription factor represses the HPV E6 Promoter by displacing SP1 and TFIID from the HPV E6 Promoter. Information. Seminars in Immunopathology. Volume 42. Ages 159 to 171. 2020.
HPV E2 disrupts TFIID ability to integrate into its integration loci within the TATA Box region, while transcriptional repressor proteins such as SP1 integrates into the HPV viral long control region to inhibit transcriptions, thereby participating in a switch that causes HPV to move from Lytic activity to repression although it is not clear if this constitutes latent status. This activity occurs in the P97 promoter and causes typical downregulation of oncology promoting expression of E6 and E7 proteins of HPV. E2 exhibits four integration loci in the P97 promoter region of HPV LCR, an early promoter compared to the late promoter in the open reading from of the E7 HPV protein in the LCR. There may be protein specific early and late promoters in the LCR for each HPV protein and differentiation of characteristics of an HPV protein can be caused by transcription initiation at loci linked to the different promoters. Information. Future Microbiol. Volume 5. Number 10. Pages 1493 to 1506. PMID 21073310.
Heparin inhibits AP1 integration into the LCR of HPV type 18. The literature confirms an oncology inhibition and viral inhibition role for Heparin with regard to AP1 and HPV in particular. Again, the repression or ‘near latent’ status of HPV seems to clearly be linked to persistence of HPV, but the lytic status with regard to upregulated HPVE6 Protein and HPVE7 protein seems to be the mechanisms by which oncology is potentiated by HPV. Heparin increased the percentage of G2/M phase cellular entities. Information. BMC Oncology. 8th Month, 31st Day, 2006. Volume 6. Number 218. PMID 16945153. Information. Future Microbiol. Volume 5. Number 10. Pages 1493 to 1506. October, 2010. PMID 21073310.
The SP1 function in HPV disease is interestingly complex, unless the drosophila cellular experimental context, which is devoid of SP1, is considered in context of HPV. SP1 in the SP1 factor free environment of drosophila cellular entities, displaces other SP factors such as SP3, while SP3 downregulates SP1 transactivation and integration into genome. This paradox occurs in genome locations for Keratin version as well as E Cadherin. Similarly, SP1 expression is increased in tissues in which HPV transcription is possible, although SP1 is not upregulated in tissue in which HPV cannot exhibit transcription. This antagonistic interaction between SP1 and SP3 was observed in HPV16 conditions, although these suggest an antagonistic interaction occurs also during pioneering development as well as regenerative as well as repair conditions. Information. Virology. Volume 224. Number 1. Pages 281 to 291. October, 1996.
SP1, SP3 and SP4 are correlated with oncology with SP1 being an indicator of oncology. The data suggests that it is the inflammation and transcriptional cascades that cause disease such as oncology, although these can begin with exhibition of a pathogen or pathogenic status. The role of SP1 has emerged as a transcriptional repressor that does not typically alleviate disease but promotes transcriptional repression that can include repression of viral transcription in a way that promotes latency. Tolfenamic Acid deteriorates SP1, SP3 and SP4, as well as inhibits VEGF. J Natl Oncology Inst. Volume 98. Number 12. Pages 855 to 868. 6th Month, 2006.
REST is a direct inhibitor of SP1 at the SYN1 promoter in tissues other than neuronal tissue although once differentiation of neuronal cellular entities occurs, there is a decrease in REST and stabilization of SP1 at SYN1 promoters. Information J Biol Chem. Volume 288. Number 5. Pages 3227 to 3239. February 2013. PMID 23250796.
AP1, SP1, Homocysteine, iNOS and s adenosyl homocysteine are all causally link to the viral vector linked to the epidemiological patterns of 2020 and 2021.
AP1 should be considered along with the MAPK, PI3K and Wnt status in the neoplasm or oncology microenvironment. Inhibiting these or modulating these in the microenvironment can result in even more substantial therapeutic effect by affecting the AP1 cascade directly. Information. Neoplasms. Basel. Volume 11. Number 7. Page 1037. July 2019. PMCID 31340499.
AP1 is a transcription activator and immune checkpoint regulator, activating PD1 and PD L1 transactions, but also can have its cascade modulated to modulate immunological checkpoint function.
AP1 is interesting because it is linked to pervasive oncology and inflammation because it is a transcription factor that can also be activated by FOX original anatomical programming pathways and includes Wnt in its pathways, clearly being included in original anatomical development pathways. A study in this research compendium clearly revealed that AP1 inhibition caused cellular entities to regress from a diseased status to near embryonic or tissue level differentiation exhibited by healthy or typical tissue as well as including some nuances of stemness.
Another study observes that in oncology of tissues of the breast, some phenotypes or some areas of neoplasm exhibit high levels of AP1 integration and high levels of AP1 transcriptional activity while others exhibited high levels of integration along with low transcriptional activity. Clearly, the post translational modifications of AP1 cascade would be involved in this. AP1 complexes, in some instances, were found to integrate into activation loci, but not cause transcription activity at all. A dominant/negative version of one of the AP1 dimers, cj protein molecule, inhibited AP1 transactivation in experimental and oncology of breast studies, while also preventing AP1 cascade from upregulation transcription in the AP1 interactive pathways. Colony exhibition was also inhibited by the dominant/negative cj molecule along with prevention of proliferation of oncology of the breast. Information. Mol Carcinog. Volume 15. Number 3. Pages 215 to 226. March 1996. PMID 8597534.
The relevancy of Nanog, then, emerges as it, along with AP1, increase the expression of E6 and E7 or HPV types 16 and 18 to enhance or, in some of the literature, constitute risk for oncology resultant of HPV. Occluding HPV18 integration loci for Nanog remarkably downregulated transcriptional activation of HPV while overexpression of Nanog without occluded integration loci increased the integration of Nanog, increased integration of cj moiety of AP1 pathways, as well as enhanced transcription of HPV.
Pivotally, a review of the integration loci for Nanog in the HPV LCR revealed that Nanog integration Loci occurred only in the in those HPV types that were causal of oncology. Information. Viruses. Volume 13. Number 8. Page 1482. July 28, 2021. PMID 34452350.
The analysis becomes more interesting. Nanog, along with OCT4 and SOX2, coordinate to maintain embryonic stem cellular entities in an undifferentiated status, such that Nanog mRNA are only found the epiblast, but minimal levels are ascertainable in reproductive cellular entities, although fibroblasts involved in extracellular matrix, connective tissue and wound healing maintenance, repair and regeneration also exhibit low levels of Oct4, SOX2 and Nanog mRNA. Fibroblast growth factor 2 FGF2 is essential in stimulating Nanog Nanog expression. Breast, ovarian, cervical and renal oncology are typically inclusive of Nanog expression.
Parthanatos is a version of cellular deterioration or a version of apoptosis which occurs when PEMT is inhibited, P53 becomes automatically upregulated, followed by P53 inhibition of pentose phosphate pathway to reduce availability of pyruvate while also inhibiting the pentose phosphate pathway at the same juncture which glycolysis is inhibited, glucose 6 phosphate dehydrogenase. The inhibition of the Pentose Phosphate pathway causes about 60 percent or more decrease in NADPH as well as impairs throughput of five carbon sugar synthesis that is linked to production of nucleotides. Resultantly, the 1 million or more instances of DNA repair that can occur in any or all cellular entities each day exhibits inadequacies of nucleotides and substrate to conduct genomic repair. This cause PARP to attach loci of genetic impairment and signal persistently until enough nucleotides and other substrate are recruited to the same locus by PARP catabolism of NAD+ to remove the ribose, followed by attachment of the ribose to local molecules. This attachment of ribose causes a gradient upon which molecules for repair are recruited and produces nicotinamide products that require nicotinamide methyltransferase to attach detoxify by attaching methyl groups to the nicotinamide, resulting in production also of homocysteine at increased levels. The pauses and incomplete performance of genetic repair results in incomplete repair and exhibition of nonhomologous repair because adequate levels of NAD+ are required to enable PARP to disassociate from the repair locus to allow Homologous Repair or error free repair to occur.
The required levels of NAD+ become so substantial that pyruvate is directed away from the diverse other pathways for energy synthesis and metabolism, as well as away from protein synthesis, toward, instead, lactate because NADH and Pyruvate are used by lactate dehydrogenase to produce NAD+ and: Lactate anion. The levels of genetic repair required, thus, can cause NADH and pyruvate to become commandeered. This process causes inhibition of glucose 6 phosphate at even more substantial levels because NAD+ is required by glucose 6 phosphate. This also causes levels of s adenosyl homocysteine, a primary inhibitor of PEMT, to increase because s adenosyl homocysteine hydrolase that produces homocysteine from s adenosyl homocysteine also requires NAD+. Homocysteine generally inhibits PEMT and increase BAX which causes cellular entities to spontaneously exhibit apoptosis although when the mitochondrial membrane is separated from the endoplasmic reticulum, the mitochondrial membrane chaperoned apoptosis pathways cannot be completed. Resultantly, a version of apoptosis occurs which is presented as parthanatos. Parthanatos is characterized by deterioration or apoptosis of already completely differentiated cellular entities along with exhibition of pluripotent cellular entities that emerge in a somewhat immortal phenotype, which eventually cause change of tissue toward oncological susceptibilities although these may enable resilience in the immediate context.
A review of the literature presents voluminous information that confirms the role of Nanog, Sox, OCT4 and UITF1 in this parthanatos context. PARP1 is A regulator of SOX2. FGF/ERK cause PARP to polyADPribosylate itself, producing a PARP/SOX2 enhancement cascade. PARP1/SOX2 integration excludes OXT4/SOX2 integration. This suggests that FGF or FGF2/ERK signaling enhance SOX2/PARP1 complex synthesis. SOX2/PARP1 complexes exhibition resultant of FGF2 or FGF balances stemness compared to differentiation. LIF and BMP4 maintain stemness even through cellular entity propagation without exhibition of differentiation. SOX2 integrates, along with OCT4 cooperation, into OCT/SOX enhancing genetic loci and promoters. OCT/SOX promoters occur in FGF4 and Nanog transcriptional regions or promoters, as well as in UTF1, SOX2 and OCT4 promoter regions. OCT4/SOX2/Nanog complexes both repress and activate transcription to maintain stemness. This nuance describes how PARP upregulation and signaling promote stemness but also results in upregulation of homocysteine that produces canonical apoptosis pathways that cause completely differentiate cellular entities to exhibit parthanatos modality of apoptosis as well as result in a persistent stemness in emerging pluripotent stem cellular entities that involves also upregulation of homocysteine such that in response, a cellular entity must exhibit strong pluripotency or escape apoptosis by upregulating BCL2 and inflammation pathways for survival such as proteolysis, S1P, S1P receptor upregulation, G Protein upregulation, all of which are linked to GSK3B upregulation. Upregulation of choline kinase and upregulation nSMase/aSMase produces phosphocholine which assist in survival pathway activation. Eventually, these conditions produce a stochastic potential for dissociation of the mitochondrial associated membrane which isolates Mitochondrial PEMT2 from endoplasmic reticulum supply of Ca2+, Phosphatidylserine and Phosphatidylethanolamine, although PI3K also sequesters Ca2+ away from the Mitochondria, resulting the characteristics obliteration of PEMT that accompanies, typically, oncology and disease. Information. Proc Natl Acad Sci U S A. Volume 109. Number 10. Pages 3772 to 3777. March, 20212. PMID 22362888.
The context presents that resultant of FGF/ERK signaling, PARP PolyADPRibosylates itself and this self PolyADPribosylation enhances its completeness or duration of interaction with SOX2, such that SOX2 is less availability to complex with FGF4.
Nanog is correlated with pathogenic oncological transitions that enable movement or migration. TWIST1/BMI1 activation by Nanog may be an essential activator of pathogenic oncology migration.
Another pivotal observation in the literature is a comprehensive confirmation of the observations made in this compendium of research. NANOG transcription activation occurs when P53 mechanisms of control are suppressed, while P53 is known to be upregulated when PEMT expression and catalysis is impaired or inhibited. These explain, clearly, why inhibition of PEMT causes upregulation of PEMT and when P53s suppression of a number of pathways, such as pentose phosphate pathway and glycolysis, becomes surmounted, a condition known as aerobic glycolysis occurs in which differentiation and proliferation of a cellular entity becomes commandeered by pathogens or pathogenic conditions to produce disease. Essential to emergence, persistence, progression, imparting of detriment, eluding of immunology and eluding of therapeutics by such disease is the dissociation of the endoplasmic reticulum from the mitochondria, preventing the ability to exhibit mitochondrial rescues pathways including programmed exhibition of cellular deterioration. Information. Oncology Biol Ther. Volume 17. Number 1. Pages 1 to 10. January 2016. PMCID PMC4848008.
The list of factors in the core list of cytokines to manage are presented in the Care Artifacts at the translationalwellness.com website. The ancillary cytokines or factors to manage are presented also in this area of the website.
However, it is important to understand that G4 quadruplex catabolism or destabilization from telomere attrition and the canonical factors that enable viral latency, are the core factors required in all disease. These including inhibition of PEMT, choline deficiency, methyl group deficiency, and homocysteine above 6 or 7 micromoles per liter, as well as s adenosyl homocysteine above 0.012 micromoles per liter.
CRISPR perfect gene editing has already demonstrated the ability to eradicate HIV and eradicate HPV, but the translation of these to implementation is obviously less than optimal for those affected by many diseases, including the viral vector exhibited in the pandemic of 2020, 2021 and incipient nuances of 2022. There has been no mention of CRISPR in application to alleviate numerous viral vectors which are challenged to assured health among human populations. It is recommended that communities and groups and philanthropies begin to understand the assertions presented in the translationalwellness.com care artifacts and begin producing therapeutics, drugs, and supplements that assure human priority, particularly by focusing on those therapies which are known gaps, and which are unlikely to be brought to market in a timely manner.
The factors here suggest that therapeutics should, today, be able eradicate all viral disease and all microbial afflictions. The information presented in this context suggest that HPV, diverse oncology, HIV, HSV, EVD/EHF, and many other disease, particularly viral and microbial disease, may be prevented and eradicated now using factors that are already in the market including natural, nutraceutical or other factors.
The Translational wellness care artifacts are important to understand. These are described in the following.
Level 1 presents the core factors that are causal or caused by pervasive detrimental health statuses and human outcomes.
Level 2 provides an expanded set that are caused by core indicators which cause core indicators, generally.
Level 3 will be described after level 4.
Level 4 is a derivatization of the observation that pervasively and generally, core indicators cause the inhibition of the enzyme PEMT, upregulated P53 to make it susceptible to pathogens or disease which subvert the function of P53, along with the upregulation of Homocysteine and s adenosyl homocysteine that immediately results from inhibition of PEMT. Level 4 presents direct capabilities and pathways to inhibit homocysteine in its diverse manner of exhibition.
Level 3, the care artifact, present an example of how to map a disease, health status, symptom, behavior or human outcome, as well as a toxic factor, detrimental influence or other detrimental factor to the core indicators and ancillary indicators which factor utilizes to cause detriment to human physiology, cognition and behavior.
The level 3 expanded information set is being developed in software capability. This capability will look at the 130 or more factors and review the data as well as the literature to present which of the 130 indicators are essential and causal, essential but not causal, correlated and causal, correlated but not causal as well as inversely associated to the disease. Importantly, disease, pathogens or conditions utilize the core indicators to emerge, persist, progress, impart detriment, and elude physiological capabilities as well as elude therapeutic capabilities.
Level 5. Level 5 will be constituted of a document which exhibits particular health statuses or detrimental factors along with which indicators are used by or cause such health status or detrimental factor.
Importantly, the first four conditions analyze have caused an intricate understanding of the disease included in the analyses and have presented the disruptive precise mechanisms by which diseases emerge, persist, become latent and elude immunological, therapeutic and other capabilities. The analyses thus far suggest that curative outcomes may be pervasively eluted when analyzing any disease or factor using the 130 or more indicators to understand how the condition or disease functions. Some instances are demonstrating exactly how to develop the curative or eradicative therapy, other instances exhibit that such conditions might not ever have emerged or become a socially detrimental vector if the indicators had been applied in analysis to a derivative outcome as soon as the indicator was discovered, and in other instances the analyses are revealing foundationally disruptive understanding of the condition.
Clearly, the analysis producing level 5 of the translationalwellness care artifacts is presenting the core cause of existing human disease, detrimental nuances of aging and detrimental human outcomes as being the result if impaired or hindered translational mechanisms by which data, analysis, outcomes, new discoveries, research, visualizations, insight and understanding are being translated into capabilities, processes, directives or nuance of care.
The information provided here demonstrates what translational medicine is and presents what the translationawellness.com website accomplishes.
The information here is somewhat unremarkable because there countless articles presented by the impressively expansive reach activity by systems and industry. However, as important as specific factors that are sure to inhibit, eradicate or prevent disease and pathogenic affliction seem like adequate exit points, these are decidedly inadequate. What is most important is the understanding of a mechanisms by which disease occurs, although the factors that inhibit, eradicate or prevent detrimental status regarding such a factor in disease are not unimportant. Knowledge of these factors in disease enables these to be tracked through the causal linkages to the most empirical and incipient causality, include this empirical causality in lists along with deriving natural and pharmacological therapeutic activities, natural factors, pharmacological factors, procedures or activities.
These lineages of causality may be useful in the diagnostic and analytical phase of care, but the empirical causalities in each lineage or stack of causally linked factors represents a bolt on point for therapeutics development, care processes, self help activities, natural therapies, or changes to lifestyle and environment. Also, these produce bolt on points for statistics, data science, correlates, policy synthesis, analytical lenses or contexts.
Translational wellness analytically derives these to empiricism and considers the wholistic factors that affect the empirical factor or which are affected by such empirical factor, including the causally linked stack by which any factor becomes linked to such empirical factor. Translational wellness then provides these factors as vectors that affect or determine quality of being, quality of cognition, and duration of being.
It is important to know that volumes of patents and research exist that provides enough information already to prevent almost every detrimental outcome. Civilizations will have to commission their own development organizations and initiatives, acknowledge that indefinite duration of optimal being is worth funding through population level collective funding, or investments into organizations that specifically produce therapies that are focused, of diminished volume and which eradicate disease must be made by philanthropies, organizations and systemic entities. Tracking therapies that should have been translated into care capabilities as well as tracking detrimental factors and influences in civilization, must become priorities and are complimentary.
The viral vector linked to the epidemiological patterns of 2021 and 2022 imparts at least some of its pathology through iNOS expression. It should be presented also that viral vectors typically utilize iNOS to deactivate the immunological system and impart increasing levels of pathology similar to most if not al diseases when these become most detrimental to outcomes. Melatonin and curcumin inhibit iNOS similarly to curcumin and some studies present melatonin as well as nitric oxide instrumentation to replace and enhance that which would be provided by functional iNOS, eNOS or nNOS, is a significant therapy to improve outcomes from the viral vector linked to the epidemiological patterns of 2020 and 2021.
Information. FASEB J. Volume 12. Number 9. Pages 685 to 693. June, 1998. PMID 9619447.
Information. Life Sci. Volume 250. Number 117583. 6th month, 2020. PMID32217117.
Information. Food Sci Nutr. Volume 8 Number 10. Pages 5215 to 5227. September, 2020. PMID 33133525.
Curcumin inhibits Herpes, HIV , influenza a, HPV, hepatitis and other viruses, for a number of reason, although inhibition of iNOS is a central factor. Information. Plant Medicine Research. “Curcumin from turmeric inhibits zika, HIV, Herpes, and other viruses”
Curcumin impairs replication of HIV1 and HIV2 and prevents HIV traversal of the genital mucosal epithelial barrier. Turmeric curcumin inhibits entry of all Hepatitis C variants into human hepatic cellular entities. Basant Polyherbal cream with curcumin, reetha, amla, aloe vera, as well as curcumin alone produce increased rates of clearance of HPV cervical affliction with basant polyherbal cream producing 83 percent clearance compare to placebo 73 percent and curcumin individually producing 81 percent clearance compared to 73 percent placebo. Enveloped viruses generally are inhibited by curcumin and this disruption included disruption and leakage of liposomes used to encapsulate viruses, confirming that curcumin disrupts the escape of viral vectors from the plasma interstitial space that is enabled by iNOS and phospholipase D as well as phosphatidylcholine specific phospholipase C in which viruses escape into the intracellular spaces in endosomes produced from phospholipase D budding and iNOS production of escape conditions. These also explain similar process which might be occurring in the lumina or lumen. Plaque formation from enveloped viruses was inhibited by curcumin also. Influenza, vaccinia, herpes, hepatitis c, coxsackievirus B3, and other viruses were assayed among enveloped viruses with a therapeutics response that inhibited PI3K, PKB, MAPK, hemagglutinin, nf kb, UPS ubiquitinases and other factors. HIV1 integrase, Hepatitis B virus PGC1 alpha, Influenza virus pathology aggregately, and Influenza viral haemagglutination activity, all are inhibited by curcumin in particular.
Information. Virology. Volume 373. Volume 2. Pages 239 to 247. Information. Food Chem. Volume 119. Pages 1346 to 1351. Information. FEBS Lett. Volume 584. Volume 11. Pages 2485 to 2490. Information. Biochem Phamacol. Volume 49. Number 8. Pages 1165 to 1170. April, 1995. Information. FEBS J. Volume 280. Number 22. Pages 5829 to 5840. November, 2013. Information. J Natl Med Associ. Volume 88. Number 6. Pages 333. 6th Month, 1996. Information. Food Funct. Volume 6. Number 11. Pages 3412 to 3419. November, 2015. Information. PLoS One. Volume 8, Number 5. Pages e62482. May, 2013. Information. Asian Pac J Cancer Prev. Volume 14. Number 10. Pages 5753 to 5759. Information. Gut. Volume 63. Number 7. Pages 1137 to 1149. July, 2014. Information. PLoS One. Volume 10. Number 4. Pages e0124903. April, 2015. Information. Volume 10. Number 6. Pages 27539. 6th month, 2016. Information. Antiviral Res. Volume 142. Pages 148 to 157. 6th month, 2017.
Glycolic acid is used as the basis to which other factors are integrated in production of viral adjuvants, particularly then the viral particles exhibit glycoprotein envelopes. Glycolic centered nanoparticle encapsulated inactivated porcine reproductive virus and porcine respiratory virus produces a an effective comprehensive protective response in porcine populations. Glycolic Acid inactivates reptilian venom activation of PI metalloproteinase, and prevents BaP1 from causing enzymatic, hemorrhagic and edema conditions. Acquired epidermodysplasia verucciformis or EV and AEV linked to HPV viral conditions can be improved by Topical Glycolic Acid, Cidifor, HPV 9 valent vaccine, Acitretin, topical imiquimod, topical retinoids, cellular immunity improvement or changing transplant medication to mycophenolate mofetil. This present clearly that glycolic acid, or methylthioglycolic acid may participate in viral protein proteolysis, tissue resection and desquamation, and in generally xenobiotic response as strong antihistamine. These present some of the ways in which withholding of dimethylacetothetin, sulfur deficiency and inactivation of thetin homocysteine methylpherase has been detrimental. Flat warts may be cleared using Glycolic Acid Lotion, as verified by clinical studies of 100 percent clearance among all patients. Information. J Clin Aesthet Dermatol. Volume 4. Number 9. Pages 62 to 64. September, 2011. PMCID PMC3175803. Information. Toxicon. Volume 71. Pages 41 to 48. September, 2013. Information. International journal of Nanomedicine. Volume 9. Number 1. Pages 670 to 694. January, 2014. Information. Vaccines (Basel). Volume 9. Number 4. Pages 310. 4th Month, 2021. PMID 33805880.
Information. Int J Dermatol. 8th Month, 2021. PMID 34403500. Information. Medscape. Article 750286.
Curcumin exhibits antibacterial activity toward staphylococcus versions, pseudomonas and streptococcus versions. Information. Front Microbiol Volume 10. Number 912. 2019. PMID 31130924.
Catechin and Curcumin integrate with S protein and host receptor ACE2, both essential aspects of pathology and cellular access for the virus linked to the epidemiological events of 2020 and 2021, as well as integrates with the S Protein after it complexes with ACE2, the fusion point for the viral vector’s access to the cellular environment. At least one study recommends catechin and curcumin as a therapeutic strategy for the viral vector linked to the epidemiological events of 2020 and 2021. Information. Scientific Reports. Volume 11. Article 2043. 2021.
Curcumin prevents pneumonia from advancing to levels which are detrimental to vital being as well as downregulate Acute Respiratory Distress Syndrome by inhibiting the Nf kB Inflammasome. Information. Heliyon Volume 7. E06350. 2021.
Favipiravir exhibits improved outcomes among those receiving care for the viral vector linked to the epidemiological patterns of 2020 and 2021. Transfer of the HSV Thymidine Kinase protein into HPV16 cellular entities sensitizes these cellular entities and produces 85 to 90 percent level of apoptosis when exposed to Gancyclovir or Acyclovir. Information. Hum Gen Ther. Volume 14. Number 1. Pages 45 to 47. January, 2003.
Probiotic usage increases chances of HPV clearance by about 50 percent. These clearly present inflammasome, iNOS, trimethylaminenoxide, phospholipase D, phosphatiylcholine specific phospholipase C, inhibited PEMT and other factors are important in enabling HPV viral conditions to emerge, persist, progress, impart detriment and elude physiological and pharmacological capabilities. Information. Eur J Cancer Prev. Volume 22. Number 1. Pages 46 to 51. January, 2013. ‘’
A study of emerging oncological conditions in the cervix implemented a vaccine that can be instrumented after affliction by HPV, resulting in as much as 36 percent of those exhibiting emerging HPV oncology in the cervix becoming cleared of such affliction and cleared HPV Viral affliction. The therapy is known as Tapkinogen or Sovacivec. Information. Gynecologic Oncology. 4th month, 4th Day, 2019.
HSPe7 immunotherapy remarkably reduces warts in HPV affliction. Information. Diseases of the Colon and Rectum. Volume 45. Number 4.
Photodynamic Therapy using theta aminoleulinic acid was utilized to eradicated pathogenic oncological lesions in 83 percent of participants, cleared HPV affliction in 80 percent of patients whom were exhibiting oncology, regressed 57 percent of patients with oncology. Information. Volume 93. Number 5. Pages 1269 to 1275. October, 2017.
Ubiquitination of P53 by HPV E6 protein linked to AP protein to produces a E6/AP/P53 complex, results in proteosome deterioration of P53 to produce enhanced risk in HPV conditions. P53 can often be a focus for pathogens and pathogenic factors because P53 promotes apoptosis or senescence that can disrupt pathogenic processes. Cervical carcinoma resultant of HPV can be regressed and prevented using the small molecule E6 inhibitor NUTLIN as well as NSC 652287 5,5’-(2,5-furandiyl)bis-2-thiophenemethanol, both inhibit MDM2 enabled ubiquitination of P53, rescuing deterioration of P53 that is required for many diseases, HPV oncology enabled by E6/AP/P53 complex. Information. Cat. No. 2443. Products. Tocris.com. Information. Pubchem CID 374536. Information. PLoS Comput Biol. Volume 10. Number 12. Article e1003991. 2014. Information. Open Virol J. Volume 5. Pages 80 to 95. 2011. iNOS levels are correlated with high risk HPV viral vectors and prognosis. Information. PMID 22420338. Carrageenan is effective as therapy for HPV viral disease while Curcumin also promotes cytotoxicity to cervical oncology linked to HPV viral conditions, particularly through inhibition of Inducible Nitric Oxide Synthase. Information. Sex Transm Dis. Volume 48. Number 7. Pages 458 to 465. Pages 458 to 465. July 1, 2021. PMID 33433173. Information. Mol ‘Cellular’ Biochem. Volume 325. Number 1 and Number 2. Beginning with Page 107. 5th Month, 2009. PMID 191910010. Information. Biochimie. Volume 83. Numbers 3 and 4. Pages 311 to 318. March and April, 2001.
HPV viral conditions present the ability for a discernibly linked pathology emerged from the Viral vector. HIV is high correlated with iNOS expression and both expression of iNOS and uncoupling of iNOS, presented in studies, is required for continuous exhibition of HIV pathology. The HIV protease inhibitor Saquinavir fused to Nitric Oxide which is the product of coupled nitric oxide production, results in powerful cytotoxicity toward melanoma. LNAME was also powerful in its ability to deteriorate melanoma. LNAME is an inhibitor of iNOS and nitric oxide is the produce of coupled or unimpaired nitric oxide synthase catalysis. Clearly, inhibition of iNOS should be integral nuances of therapy in viral conditions including HPV, HIV, and even respiratory viral vectors such as that which is involved din the epidemiological events od 2020 and 2021. Of the diverse viral vectors reviewed by this compendium of research, iNOS was required to be modulated in some way by each of these viral vectors. Information. Oncol Rep. Volume 28. Number 2. Pages 682 to 688. 8th Month, 20212. PMID 22665020. Information. Med Res Rev. Volume 40. Number 1. Pages 158 to 189. Jan 2020. PMID 31192483.
Inhibitors of Phospholipase D are also recommended because the combination of iNOS and Phospholipase D enables viral vectors being impaired by the reactive molecular species in the plasma membrane interstitial space to escape in in endosomes to become exhibited in the cytoplasm. Protection from wireless fields, communications fields, electricity fields, and atmospheric particular are also recommended during the therapeutic period. HPV is known to be upregulated by HPV 16 E7, promoting resistance of HPV to rapamycin that is correlated with pRb status.
iNOS and HPV are features of environmental wireless communications, electricity fields that are unshielded, and atmospheric particulate, while diseases linked to HPV or other viral vectors are enhanced because strong electromagnetic fields enabled iNOS and phospholipase D express in the epithelium and endothelium of lumina which are enclosures deep in tissues that are intended to be shielded from electromagnetic energy by the architecture of physiology. Phospholipase D upregulates phosphatidylcholine specific phospholipase C which deteriorates the most abundant phospholipid in cellular membranes and physiology, as well as deteriorates the pulmonary surfactant dipalmitoyl phosphatidylcholine which is essential to easing surface tension in the alveolar lumina of pulmonary tissue to enable improved exchange of Oxygen and exchange of CO2. Information. BMC Oncology. Volume 18. Number 1. Pages 485. 5th Month, 27th Day, 2018. Some pathogens emit their own phospholipase D which then perform catabolism of dipalmitoylphosphatidylcholine.
A new way of producing iNOS inhibitors is presented in this study of anchored plasticity inhibitor design. Nature Chemical Biology. Volume 4. Pages 700 to 707. Pages 2008. October 12, 2008.
Berberine completed inhibits 6 tested HIV1 isolates. Berberine in Obatoclax both individually inhibit the viral vector linked to the epidemiological events of 2020 and 2021 at low molecular levels. Berberine suppresses HPV Viral vectors, and causes apoptosis and abated development in cervical oncology resultant of HPV. The literature is considering presentation of berberine is a broadly active antiviral. The mechanism of action for berberine activity is presented as inhibition of AP!, but berberine is active in inhibiting a number of essential inflammatory cytokines required in diverse pathology. However, to summarize, most of the factors presented in therapeutic lists within the translationalwellness.com material produce beneficial affect to oncology, disease and other detrimental outcomes when these factors are prevented or alleviated. Information. AMB Express. Volume 10. Number 1. Page 164. September 8, 2020. Information. “Berberine and Obatoclax.” Viruses. Volume 13. 2020. Information. FASEB J. Volume 35. Number 4. Article e21360. 2021. PMID 33749932. Information. “Berberine modulates AP1”. Molecular Cancer. Volume 10. Number 39. 2011.
This discussion thread includes some discussion of viral vectors for disease, including those potentiating oncology. A relevant context is presented here.
Folate receptors are upregulated by elevated homocysteine, and are a feature of pathogenic oncology and can occur in typical cellular entities. Folate receptor synthesis upregulation can occur in pathogenic conditions although in some oncology, such as cervical oncology, such upregulation is not regressed once folate adequacy is achieved. Such folate receptor upregulation occurs without required upregulation of folate receptor mRNA or upregulation or an increase in hnRNP E1. Homocysteine upregulation was coordinated with Folate Receptor upregulation. Folate receptor inhibition may be therapeutic in cervical or other oncology to counteract persistently upregulated and overly persistent Folate Receptors. Impaired ubiquitinase activity, modulated proteolysis as well as changed autophagy may also explain overly persistent folate receptor activity. J Clin Invest. Volume 113. Number 2. Pages 285 to 301. Jan, 2004. PMID 14722620.
The literature presents that In Vivo delivery of CRISPR/CAS9 focused on excision of HPV E6 and E7 genetic structures using pegylated liposomes results in complete regression and disappearance of neoplasms and results in 100 percent survival of experimental study participants or subjects. The gene editing was largely linked to NHEJ compared to high fidelity homologous repair, but this could be a result of large gene editing payload, although the neoplasms disappeared through apoptosis suggesting that cellular and humoral immunity as well as cellular decision mechanisms were extremely efficient at removing neoplasm or oncology once HPV E6 and HPV E7 genetic sequences were excised. Protein transduction therapy is field that has emerged and mature in developing protein domains that enable large payload biologically active molecules to be moved into the intracellular environment where intracellular chaperones reshape the payload into biologically active quaternary structure to resume shape, twist, writhe and reactivity characteristics. Linking CRISPR/CAS9 to transduction domains should allow the removal and deactivation of every known pathogen from human biology and should be able to cause the disappearance of every known oncology by excising or repairing the required genetic factors, typically numbering more than 1000, in oncology. Protein transduction domains enable large molecules to permeate cellular physiology with 100 percent coverage and the efficiency of a water molecule’s permeability of cellular physiology. Information. Mol Ther. Volume 27. Number 12. Pages 2091 to 2099. December 4, 2019. PMID 31537455. Information. Gene Therapy. Volume 8. Numbers 1, 2, 3 and 4. 2001. March, 2001.
CRISPR/CAS9 has already completed eradicated HIV in small nonhuman mammals in 2013. Information. Nature Communications. Volume 10. Article 2753. 2019.
A most important observation in this context seems to be that in the context of translation wellness achieve by translational medicine, CRISPR/CAS9 along with protein transduction domains, potentiates rapid translation or reducing of discoveries and insight in biology and therapies, as well as disease and regenerative medicine into practice using personalized groups of interventions. Simply, not only is it possible to devise a combination therapeutic or groups of therapeutics for an individual, but using proteomic decision which CRISPR has already demonstrated, each cellular entity in physiology can have an individual care plan.
This data is presented in one of the wellness artifacts at translationalwellness.com
continuing research and develop is occurring at translationalwellness.com. There, they are translating this information into usability competent tools, technologies and empirical conclusions as well as guidance for providers, practitioners, patients, systems and industry or other organizations.
continuing research and develop is occurring at translationalwellness.com. There, they are translating this information into usability competent tools, technologies and empirical conclusions as well as guidance for providers, practitioners, patients, systems and industry or other organizations.
The most important conclusion here is that the translated wellness indicators of the amehsi specification now present the empirically causal factors of aging and pervasive disease. These should help any clinician begin introducing stabilizing and regenerative care pathways that included alleviate and eradicating the cause of detrimental factors in aging. The amehsi websites and translationalwellness websites all provide information that clinicians, practitioners and consumers can be review and understand, particularly because these include both pharmaceutical prescription and nonprescription, natural, nutraceutical capabilities. The systemic factors that diminish vital being are only presented here because these seem to be being imposed by systems in a way that humans should understand and be aware of.
Clearly, there is something inadequate presented here. These represent some among many ways in which any system of the universe, or any system of civilization, has the inherent propensity to prioritize itself over its incipient purpose, incipient utility and over humanity.
These all present the manner in which workers in systems prevent systems from annihilating humanity and abrogating species. Every day the humanity continues to exist in context in systems result in consistent selection of the most detrimental alternatives and imposition of unnecessary massive detrimental outcomes among humanity
represents the service that workers in systems of civilization and workers providing service in civilization all have triumphed. Its victory that must be achieved every day. Its indication that less-than-optimal outcomes or detrimental outcomes among system workers and humans do not indicate human flaws but represent instances in which systems
have broken through the protection that people in systems provide from the inherent nature of systems to prioritize themselves over humanity.
Consider this. Ask any individual or group representing humanity the following.
If every wireless service provider contract allowing providing of wireless communications inhibits PEMT, causes iNOS, phospholipase D, phosphatidylcholine specific phospholipase C, also in the lumen, also in alveolar lumina, causes freakish biological occurrences in the lumina, is integral to massive detrimental behavior, disease and abated being, then why are these allowed to exist or occur and what must workers in systems to do counteract these?
If changes in electricity output since the 1800s inform in near perfect correlation the change in abated vital being since then, why are these allowed to occur when they can be mitigated by insulating and shielding all electricity and communications wiring or interfaces in homes, dwellings, buildings, open areas, infrastructure, devices substations as well as power generation stations while also what must workers in systems be required to do counteract these effects.
Since it is known that homocysteine and PEMT are the core of disease and causes deterioration of social function, then why do we allow these to escape being priorities in care and escape being acknowledged as priorities in deliberations regarding detrimental outcomes as well as escape being priorities in synthesis of social constructs. Why are these allowed to cause massive detrimental behavior and what must workers in systems be doing to counteract these and prevent the complete deterioration of civilization?
Since it is known that implementation of abated vital being as a sanction causes between 20,000 and 1,000,000 or more instances of abated being on one civilization alone, with similar increase caused among the world’s population, with substantial increase in detriment to system workers, massive increase in transportation mishaps, decreased span of being, and other detriment, why is this imposition of abated being continued to be utilized as sanction? As many as 550,000,000 or more detrimental outcomes are linked to 1,000,000 instances of vital being if maintaining ratios of abated being to detrimental outcomes, such that 550,000,0000 instances of detrimental outcomes each year expands beyond the capacity of civilization and becomes causal to massive geopolitical conflict and detrimental outcomes among the world’s populations. What must system workers and the world be being required to do to counteract this massive detriment.
These susceptibilities are known to harvest humans in susceptible contexts to produce massive detrimental outcomes.
Since 1906, enough economic resources have been expended on temporary solutions that allow profit or benefit to be obtained from other’s misfortunate such that, instead, a home for each familial group could have been constructed and provided freely to them. Why not just begin building homes for those who require it and allowing people to pay as they are able at costs for those homes instead of continuing allow benefit to be obtained from human misfortune? What must system workers and the world’s population be being required to do to managed or counteract these conditions?
Permanent magnet solutions allow hundreds of thousands of megawatts of free, wasteless energy production. Why are civilizations continuously selecting sources of energy for homes, infrastructure, transportation, automotive, industry, and other applications that produces massive wastes, produce atmospheric and environmental particulate/pollution, are excessively expensive, produce waste that can be used to produce massively detrimental artifacts, and cause the most massive detriment to human populations.
Why are water management solutions excluding the production of water freely from atmosphere and including doing so at the oceanic or aquatic boundaries with land to assure adequate moisture when producing water freely from atmosphere in quantities of billions of liters each day? Why are the most detrimental, invasive, environmentally detrimental solutions to water management and obtainment being selected? What must system workers and the world’s population be having to do to manage or counteract these detrimental selections?
Civilizations which do not provide adequate living wage freely to its populations that exceeds the requirements for housing, nutrition, water, health services, education, safety, stability, human condition, social condition, behavioral condition, physiological condition and the economic condition, amplify the effect of Roemer’s dynamics and cause global exhibition of Roemer’s dynamics in which human detrimental outcomes increase to satisfy the requirements of organizations and populations of the world providing services utilized to manage detrimental human outcomes. Why is a living wage not assured in such regard. What must system worker’s and Human populations be being required to do to counteract these dynamics
Thus, what is a capitalism, value synthesis in the foundational pathways of satisfying human, social, behavioral and physiological requirements or is it mere competitive grab for the modes of production and natural resources such that private interest can impose their biases, priorities and interest upon Huan population.
Thus, what is Democracy? Is Democracy a system in which any Majority is allowed to impose its biases, inadequate understanding, inaccurate opinion, opinion, and priorities on any less than majoritarian group, including imposing these detrimental decisions and contexts on populations that can be scapegoated because they are not among a majority?
What is a Republic? Is it the election of a system of laws a Ruler that operates with impunity, imposing social constructs and sanctions that result in millions of instances of abated being each year as well as 550 million detrimental outcomes each year, with similar effect to the world’s populations? Is it exclusion of biology and science from social construct synthesis and as well exclusion of these from being priorities in deliberations regarding detrimental outcomes in a way that requires humans to be acquiesce to being causal for detrimental outcomes, causing humans to believe that these outcomes emanate inherently from humanity while systems impose the conditions that deteriorate social function, neurology and foundational nuances of cognition while commandeering the cues for primitive complex resolution of these in nature in a way that assures systems that benefit from detrimental human outcomes are continuously utilized with objectives, quotas and revenue objectives that require detrimental human outcomes occur become assured?
Or, could the Golden Apple of a Democratic Republic be a priority for Life, Liberty and Pursuit Happiness with systems of civilization and Constitutions performing as the silver frame for that Golden Apple, with capitalism a modality of assuring opportunity, assuring value creation, and most efficiently and most effectively keeping Democratic Republics true to the favor of the Universes afforded to each among Humanity?
The founders of modern civilization’s systems have not ever intended to produce a static, unchanging group of institutions as the core of a civilization. Modern civilizations were intended to continuously elute information about the human condition, requiring analysis and understanding, followed by ever improving synthesis of social constructs that improve the human condition, expand liberty, and prevent exhibition of detrimental nuances of the status quo. Imposing massive levels of abated being upon populations because one thinks that are privileged to do so, because one decides to ignore science and biology, or because one exhibits biases that can only be confirmed by imposing outcomes consistent with those biases, does not constitute processes consistent with a Republic or a Democracy. Similarly, imposing a system of social constructs and deliberations that excludes biology, excludes science, ignores data, ignores mechanistic links and is designed to reserve absolute priority to such a system of social constructs itself over humanity, human vital being, Liberty and opportunity, are wholly inconsistent with the Golden Apple, the Silver Frame, and with the favor afforded Humanity by the Universes.
Western civilization’s 50 to 60 hz baseline field amplified by millions of other devices, wifi, network, wireless, electrical or other fields, as well as toxins and environmental particulate, enables luminal, endothelial, cortical and other areas to potentially exhibit PLD and iNOS, as was well as phosphatidylcholine specific phospholipase C in lumen areas of physiology which physiological compartmentalization were intended to protect from such pathogenic influences. Pulmonary alveolar compartments are lumina. Phosphatidylcholine specific phospholipase C deteriorates the phosphatidylcholine lead group of the major surfactant in the lumina and electromagnetic fields impose freakish, atypical transitions in lattice and structure characteristics linked to atypical proliferation, impairment, disease, alveolar disruption and other changes.
The year 1841, glycolate was discovered. The year 1878 in the proceedings of the royal society of Edinburgh, it was observed that Dimethylacetothetine or thetin, depleted homocysteine at 700 times the level of any such factor used even in modern medicine or until recently used in modern medicine. The enzyme PEMT integrates CH3 into anti-inflammatory fraction of phosphatidylethanolamine to produce, first, phosphatidylmonomethylethanolamine, then phosphatidyldimethylethanolamine, phosphatidylcholine. CH3 is merely attached sequentially to the three open locations ion the Nitrogen of Phosphatidylethanolamine to make phosphatidylethanolamine phosphatidylcholine. However, the Phosphatidylethanolamine, PMME, PDME and Phosphatidylcholine all are strong antihistamines and activate trypsins, serine proteases, the ‘clotbuster’ or thrombolytic Tissue Plasminogen Activator, all in a way that deteriorates proteins to foundational levels, structurally deteriorates carcinogens, deteriorates xenobiotics, and produces a clean, safe environment for development known as embryonic plasticity.
PEMT selects an enriched faction of phosphatidylcholine that has extended length arachidonate, DHA, omega-3, oleoylate, first fatty acid in fatty acid beta oxidation known as palmitate, insulated, ether linked fatty acids. PEMT attachment of CH3 integrates 1 molecule of hydride, the energy that fuels stars of the universes, compared to two molecules of hydrogen, which when adequately integrated into membranes produces a background pH of 7.2 to 7.6 required for biological function, required for conscious cognitive function and control, as well as produces a gradient when compared to circulating H+ upon which redox transitions using hydridic redox factors NAD+/NADH, NADP+/NADPH, and other redox factors occurs. This redox factors release and recapture 2 eV- as energy and fluorescent energy or light that performs the active fields in which biological activity occurs. PEMT is required to be dysregulated in disease, inhibited in disease, diminished correlation with detrimental aspects of aging, disease, detrimental behavior, behavioral health conditions, etc. Homocysteine increases when PEMT is inhibited, and homocysteine disrupts coordination at the cellular level required to produce biological systems activity. Homocysteine levels are correlated to difference susceptibility to disease and abated being between genders, differences in susceptibility and abated being between age groups, correlates directly to the statistical sigmoid use in actuarial projections that require understanding of changes in risk for abated being according to age.
Homocysteine can be depleted by Thetin Homocysteine Methylpherase using dimethylthetin, trimethylsulfonium, or other thetins, and relieves homocysteine levels from inhibiting PEMT. Sulfur deficiency causes thetin Homocysteine methylpherase to exhibit intramolecular disulfide linkages that deactivate the enzyme by producing a gel phase explaining why a homologous social outcome is so prevalent in particular civilizations. Thus, when the ability to depleted homocysteine by thetin homocysteine methylpherase was discovered, it was found that dimethylthetine and homocysteine were metabolized to produce methionine and methylthioglycolic acid. Methylthiogolycolic acid is a desquamation factor or strong antihistamine that is an inorganic to organic phase separator and transfer factor, separating biotic phases from abiotic phases and moving useful molecules from abiotic phases into biotic phases for use by biology, similarly to phosphatidylethatholamine, ethanolamine, CTP – Ethanonamine, Phosphoethanolamine, PMME, PDME and enriched phosphatidylcholine.
Methylthioglycolic acid can be placed into inhospitable, diseased, challenged, toxic environments and derivatizes or elutes molecules that would help resolve such challenged environments, in a process known as derivatization and in a process by which pervasive drugs in the 1800s and 1900s were produced. Thus, instead of managing homocysteine and assuring the function of PEMT by providing dimethylacetothetin, volumes and volumes of drugs were produced using the same methylthioglycolic acid or its derivatives which human physiology would have produced for itself if provided dimethylthetin, if PEMT function were assured or if homocysteine were managed to below 6 or 7 micromoles per liter. This is why methylthioglycolic acid or glycolic acid is known in the literature as the center of medicinal chemistry. The decision to not use dimethylthetine, PEMT management and homocysteine management prevented, beginning in 1878, the ablation of almost all disease. Instead, more ways of inhibiting PEMT and increasing homocysteine were invented including wireless, electricity, electronics, as fields, and atmospheric/environmental particulate and toxins, much of which inhibit PEMT in some way including through causing iNOS, phospholipase D, luminal expression of phospholipase D, iNOS and Phosphatidylcholine specific Phospholipase D, as well as through activation of the list of cytokines presented in these analysis as clinical indicators.
Because inhibited PEMT, homocysteine and impaired de novo synthesis of phosphatidylcholine, deteriorate the specifics specific development and sustainment of foundations of biological compartmentalization, and deteriorate brain, neurology, conditioning, recall, blocking, rewards system, memory and basis of social function and behavior in particular patterns and these patterns are resolved in particular primitive but complex ways in nature using cues, shapes, colors, smells, patterns, associations, inclinations, susceptibilities, subjectiveness and other ways that allow foods, nutrition, migration or other rescuing responses, civilizations have learned to commandeer these cues to produce outcomes that sustain systems. The result is that massive detrimental behavior and physiological outcomes are allowed to occur instead of managing Hydridic balance, foundational compartmentalization, PEMT stability assurance and homocysteine stabilization.
Even drugs pervasively increase homocysteine, iNOS or inhibit PEMT directly or competitively by competing for methyl groups.
The function of PEMT in producing PMME, PDME, and phosphatidylcholine is important in the pandemic and epidemiological climate because it is populations that have strongest PEMT function and highest fraction of maintained PEMT function who are least susceptible to complications from the viral vector of the pandemic. This is because iNOS expression is required by every virus, PEMT is inhibited correlative to age, homocysteine is increased typically in correlation to age, and phosphatidylethanolamine, PMME, PDME, and phosphatidylcholine enriched fraction all are linked to upregulated proteolysis and protein deterioration by trypsins, tissue plasminogen activators and xenobiotic response. Viral proteins and structures are proteolyzed, autophagocytosed, or otherwise deteriorated by the PEMT competent physiology. The use of proteases and proteolysis factors such as nattokinase, serratiopeptidates, and other proteases such as NATTO and others, can be utilized to assist in deterioration of viral proteins.
Since the year 1878 when dimethylthetin could have been used to manage PEMT and Homocysteine, almost every disease and detrimental outcomes could have been prevented, alleviated or benefited. A study by a prominent health services provider found that in a population of 10,0000 in which homocysteine was below 6 or 7 micromoles per liter compared to a comparative slightly lower population in which the levels above 6 or 7 micromoles per liter were exhibited, over a period of 1 decade there was 1 to 500 comparative risk for abated being from any causality, such that those exhibiting 6 or 7 micromoles per liter or lower exhibited only 1 instance of abated being while those with a homocysteine level above 6 or 7 micromoles per liter exhibited 500 instances of abated being. This suggest that by not managing homocysteine using dimethylthetin beginning in 1878, followed by the observation that no known person exhibiting vital being in 1878 now also exhibits vital being, a species for the first time in the span of the exhibition of the Universes consciously imposed the complete abrogation of all of its own species that by depriving such population of knowledge, innovation, development and care. It is important to know that homocysteine at increased levels is linked to all disease, detrimental behavior, risk for sudden adverse health events, risk for becoming a victimizer, being victimized, incurring accidents, exhibiting behavioral health conditions, or any factor linked to abated vital being of any cause including being in a geopolitical conflict.
Thus, by inventing new ways of inhibiting PEMT, a global fog of impaired neurology, cognition and physiology was imposed upon the world that resulted in the tumultuous events of late 1800s, 1900s and 2000s. Dimethylthetin was not utilized in any of the pandemics or epidemiological events. Today, there is no requirement by any civilization that the empirical cause of disease be treated or managed in health services intervention. Every practitioner, researcher, manufacturer, drug development or other factor in industries that produce toxins, managed care, produce drugs and produce research, all have a business function filters out any innovation or change that will prevent exhibition of massive abated being and massive levels of detrimental behavior. Abrogating a disease results in potential revenue decreases. Civilizations that don’t provide assured incomes to their populations, assured housing, assuring nutrition, free water, and free health services, health services that a required to treat and prevent the empirical causes of disease , as well as civilizations that allow populations to believe that individuals are causal to detrimental behavior when in fact it is these allowed deterioration of the nuances of social function and behavior along with allowed exhibition of susceptible conditions which are the true empirical causal factors for detrimental behavioral outcomes, represent civilizations that knowingly and systematically cultivate massive detrimental behavior and detrimental physiological outcomes often as a way imposing and cultivating bias, imposing and cultivating power over others, as well as produce massive levels of revenue.
The use of abated being as a sanction was paused in 1972 until 1976, resulting in 20,000 per year decrease in abated vital being among on civilization’s population alone. The trend however presented a pattern toward a 100,000 decrease within 3 years and nearly 1,000,000 or more decrease in yearly levels of abated vital being within about 7 or 8 years. Using a ration of detrimental human outcomes not resulting in abated being compared to abated vital being, this translated to a decrease in detrimental humans outcomes of 550,000,000 by the time this 8th year was reached in which a projected annual decrease of 1,000,000 instances of abated vital being might have been achieved. During the pause of four years preventing use of abated being, detrimental acts involving systems workers decreased to levels exhibited in the 1950s. Mishaps in massive transportation decreased by 75 percent. New highest ever average span of being was reached during such a pause. Each instance of abated being imposed as a sanction can produce as much as 90 million dollars in revenue. 1976 presented a conclusion to the moratorium preventing utilization of abated vital being as a sanction, regardless of the massively beneficial effect it was having to human health and safety of system workers. Most importantly, at global population levels, the same beneficial effect to increased average span of being and decreased levels of abated vital being was observed as was observed at the national level within civilization imposing such a moratorium.
Relevantly, since the 1800s when electricity became implemented in civilizations, a massive change to epidemiological patterns occurred. These include a nearly perfectly inverse correlation between change in electricity and change abated vital being among developing and adult populations, along with a nearly perfectly positively correlation beginning in 2009 after changes produced by a 2005 communications and safety act. During the closing of an embassy and exit of diplomatic personnel in 2020 to 2021, a municipalities rates of abated being from the pandemic increased immediately before and immediately after the decommissioning of the diplomatic location, clearly indicating that communications and information exchange had caused the increased levels of abated being.
here are the kinds of potentialities exhibited in the status quo.
One of the researchers here, in numerous instances, was required to accompany others for inpatient care. A group of essential clinical indicators and how to manage or alleviates such indictors was presented in numerous instances and taped to the wall as well as taped to televisions in plain view of clinicians. Each time a clinician entered the inpatient setting to provide care, the clinical indicator algorithm was discussed. Every time that a clinician agreed to manage any factor in the algorithm or allow the clinical factor to be manage by manually purchasing such management capability and bringing it into the inpatient setting, the patient stabilized and was returned to the home in stable condition.
The numerous instances of care include cardiovascular and vascular conditions as well as cardiovascular and vascular indicators. The health services facility at which these activities were conducted is now among the top cardiovascular care entities, if not the top cardiovascular care entities in the nation.
That particular researcher, regardless of such contribution, has been homeless for nearly 15 yrs.
That is what is inadequate about the status quo.
securing information flow and electron flow on web
IPv4 10.15.0.20 10.15.0.20.inaddr.arpa,
this prevents this site from being used to track and mess with contributors to the discussion
an island in the central Pacific Ocean
During days of heaviest atmospheric particulate from driving and heaviest telecommunications activity, abated vital being was systematically higher during the pandemic.
Civilizations with the heaviest foliage and lowest telecommunications, particularly wireless, coverage, the rates of abated vital being was the lowest and delayed effect of the pandemic was observed in these areas.
Areas that were massively affected by the pandemic were the areas releasing 5G or other very powerful communications systems.
Areas the exhibited the earliest control of the pandemic exhibited nearly a fourteen precent decrease in electricity usage as well as substantial decrease transportation causing atmospheric particulate.
Some of the areas of other Nations where massive detrimental outcomes from the pandemic cause primitive modalities of ceremonies to be used because of inadequate resources, all exhibited release of 5G in reasonably synchronization with exhibition of the most detrimental aspects of the pandemic.
The 2020 statistical data exhibits clearly that disease enhanced by iNOS., phospholipase D and phosphatidylcholine specific phospholipase C, as well as luminal expression of these, were increased in percentages.
The data observes that 100s of billions of dollars were being paid in licensing fees for 5G, sometimes for individual contracts. These again, present how revenue is guiding factor, along with potential profit, in why massive levels of human detriment are being allowed to occur to human populations exposed to wireless, electricity, communications, electronics, and the use of abated being as a sanction, as well as exclusion of PEMT and Homocysteine as priorities in care. These represent, perhaps, the most detrimental nuances which any organism or species of the universes have ever imposed or instrumented toward its own kind or own species. Certainly, these factors have already once before caused the annihilation of a all known members of the species which were alive at the instance in which dimethylthetin, homocysteine and PEMT were withheld from therapeutic priorities in care.
Thus, civilizations sequester away everything that is obtainable in nature for free and requires payment to obtain often exactly what was free in nature. Many instance exhibit the addition of value such as safety factors, but the example of water is interesting because the chemicals added to water such as fluorine and chlorine cause expression of iNOS. Similarly, it is easy to search for ‘free water from air’ to observe that is possible to generate billions of liters of fresh water each day directly from the air for free with no environmental detriment or waste, particularly when this is done at boundaries between land and ocean. For centuries, condensation or dehumidification processes could have been used to alleviate water inadequacy but, instead, only the most environmentally damaging, most toxic, most expense, impractical and human detriment imposing ways of managing water were chosen. Even today, water systems are omitting the production and distribution of free water and are increasing prices of water obtained at retail or wholesale locations.
Power production is also an interesting context. Massive amounts of energy production and unheard of form factor efficiencies are able to be generated with no waste, no require fuel resources, all using permanent magnet system which arrange strong magnets in patterns that produce continuous motion. Using permanent magnet solutions has been possible for centuries. Instead, civilizations have consistently selected ways of producing electricity which are the most wasteful, utilize the most resources, produce the most detrimental byproducts, are the most expensive, are the most perilous to human populations and which are the most detrimental to the environment.
Since 1906 enough financial and other resources have utilized manage homelessness by paying for temporary solutions that have done more benefit private interests than they have in producing permanent solutions for the homeless. Interestingly, if all the resources allocated to such programs and initiatives were utilized to build homes, a home for every family could have been built instead, providing permanent solutions.
It is important to understand that inhibited PEMT causes a choline deficiency by preventing endogenous synthesis of phosphatidylcholine by PEMT while also preventing integrating CH3 methyl groups into Phosphatidylcholine to produce phosphatidylcholine in an enriched fraction. The CH3 exhibits hydride in a ratio of 1 to 2 compared to hydrogen. This ratio, once densely exhibited in membrane phospholipids produces a background pH between 7.2 and 7.6 that is required for biological function and is required for conscious cognitive function, such that beginning in gestation, brain, neurological centers, rewards systems which function as way of determining detrimental compared to nondetrimental behavior, conditioning, blocking in conditioning, recall of conditioned stimuli and response pairings, and conscious capacitant fields, as well as ability of endogenous capacitant cognitive fields to resist environmentally imposed conditions, response and stimuli/response pairings all become impaired in patterned ways that systems know how to commandeer by exploiting primitive but complex associations that lead to ways of alleviating homocysteine, sustaining PEMT and alleviating cytokines such as iNOS, phospholipase D, and phosphatidylcholine specific phospholipase D which deteriorates the primary surfactant DPPC which exhibits phosphatidylcholine lead groups as well as depletes the primary membrane phospholipid phosphatidylcholine.
The lumen is the innermost areas of physiology from layer perspective, is intended to be innermost protect open areas of epithelia. A most important role of having a physiology or an anatomy is to protect the lumen from environmental detriment, including gestational circumstance which protects the emerging physiology from such detriment. Pulmonary environment exhibits alveoli and alveolar lumina are areas within alveoli that physiology is intended to protect from environmental detriment. Wireless, electricity, communications and atmospheric particulate, environmental particulate, all contribute to expression of iNOS, phospholipase D, and phosphatidylcholine specific phospholipase D which deteriorates the primary surfactant DPPC which exhibits phosphatidylcholine lead groups as well as depletes the primary membrane phospholipid phosphatidylcholine.
Every virus requires iNOS and escapes the toxic plasma membrane interstitial space in endosomes produced by iNOS, phospholipase D and phosphatidylcholine specific phospholipase C activity. Bacterial lipopolysaccharide causes expression of iNOS. Inhibition of PEMT causes expression of iNOS because P53 expression with inhibited PEMT causes massive apoptosis in way that requires increase in turgor of intracellular environments in order to counteract massive decreases in the number of cellular entities per micrometer of tissue. Many therapies causes expression of iNOS. Gravity changes or returning to earth from space causes iNOS to increase the turgor of cellular entities as a way to strengthening physiology to carry its anatomical mass. Many well-known viral vectors required iNOS expression and uncoupling of iNOS I which iNOS produces reactive oxygen species superoxide, H2O2, peroxynitrite, hypochlorite, and the cause of stroke and most pervasive cause of sudden adverse health events, complications and perioperative complications known as trimethylamine-n-oxide. Trimethylamine-n-oxide is also caused by eating meat, chicken, eggs, fish, choline dense foods, carnitine dense foods, all without a pre/post/probiotic or without a broad-spectrum antibiotic including without 33 DMB, grapeseed or fruity polyphenol exhibiting olive oil.
The pandemic has revealed that wireless and electricity fields of any nature, as well as artificial light and atmospheric particulate, all are producing constant detriment to the lumina in diverse areas of physiology including pulmonary, brain, neurological tissues and other areas. It is now known that in a process known as decellularization, cardiac, pulmonary and other organs can be removed from physiology and have all cellular entities washed from extracellular matrix, followed by reseeding with stem cellular entities to enable regeneration of organs. The regeneration of organs completes outside of physiology and spontaneously resumption of biological rhythms completes spontaneously outside of physiology. The spontaneous regeneration and spontaneous rhythms are impaired or diminished when the organs have not been removed because of inflammation factors, including iNOS, which inhibit the function of PEMT and because inadequate ornithine is exhibited along with impaired extracellular matrix, laminin, Agrin, Hyaluronan, Collagen, as well as inadequate prevention or clearing of Progerin. These are all integral factors in the causing of aging, cause of rapid aging, and are inadequately considered factors in every disease.
The factors that cause iNOS, inhibit PEMT and which cause homocysteine, all accumulate, such the already existing conditions, disease or susceptibility typically indicated increased levels of these and explain increased risk in particular groups, with particular disease, or with other factors. However, since 1880 when first electricity substations were placed into areas of the largest cities, followed by atmospheric pollution and wireless communications, particularly including electricity infrastructure that is unshielded although all electrical wiring in any area, building or substation can easily be shielded or enclosed, but are not typically shield or enclosed. Electrical plugins can be covered, communications plugins can be covered, lights can be shielded, wireless networks can be replaced with wired networking, devices can be shielded, but again these are not typically done.
Accumulation of inflammatory cytokines, choline deficiency, inhibition of PEMT, homocysteine, diminished integration of CH3 into phospholipids, bacterial exposure, viral exposure, all accumulate and explain differences in outcomes. The care setting omits protecting brain, lungs, lumina and alveolar lumina from exposure to these factors. An anecdotal example provides context. A patient presenting symptoms of upper respiratory illness instrument water diluted dimethylsulfuoxide in mouthwash, surface cleaning, as well as on a wet towel placed under the door of room and in window to allow fresh cleaned air to flow in room. Systematic turning off of internet sites, social networking, changing of addresses, changing of time zones on phones and computers, turning of communications protocols on phones and computer, configuring firewalls to specific allow only essential communications on phone and computers, resulting in continuous alleviation of symptoms lasting a few hours until symptoms resumed, followed by selection of additional internet sites and sources of iNOS. Covering power outlets, turning of television at night, all produce continuous improvement. Periodic coughing symptoms were alleviated once it was realized electrical, wireless and electromagnetic fields were activating neurological pathways for coughing in brain, causing swelling of endothelium in physiology generally, and causing inflammation of lumina, including inflammation of alveolar lumina. A review of the literature demonstrated that transient alveolar changes can be affected by electromagnetic fields, such that the literature presents freakish ameliorated development of structures and lattices in the lumina attributed to grossly ameliorated status produced by electromagnetic fields, changes to quantum nuances of gravity, iNOS expression, inhibition of PEMT, homocysteine, phospholipase d and phosphatidylcholine specific phospholipase C.
Unfortunately, internet sites in some civilizations derive their valuation from volume of users. Such sites sometimes remove the ability to delete accounts and refuse to delete accounts, as well as merely deactivated but do not delete accounts. A person trying to maintain their vital being may be thwarted and experience abated being as a result. Some civilizations have implemented GDP data protection act standards that protect individuals while other have not. Some social networks and sites have massive levels of accounts of those having experienced abated being, some of which have occurred because of the participation in the website or because the ability delete the account has been removed.
Some diseases and versions of oncology are considered to only occur in western civilization and only occur because the exposure of the lumen to electromagnetic influence, atmospheric particulate, and environmental particulate such as phthalates, C8, Teflon, and other factors that cause iNOS, phospholipase D, phosphatidylcholine specific phospholipase C, inhibition of PEMT and increased levels of homocysteine as well as inflammatory cytokines.
The exposure of brain and lumina to electrical fields and causing of coughing by activating neurological pathways of causing, stimulating swelling of epithelia, and causing pulmonary lumina pathology including depletion of surfactant, all of causal factors. Utilization of proteolytic factors such as natto, serratiopeptidase, nattokinase, other versions including NATO can help deteriorate viral proteins. Enabling the function of PEMT by inhibiting homocysteine activates PEMT and allows phosphatidylserine, phosphatidylmonomethylethanolamine, phosphatidyldimethylethanolamine, and enriched phosphatidylcholine exhibiting DHA, omega-3, oleoylate, and palmitate, ether linked, and extended arachidonate fatty acids, all activated resolvins, nueroprostanes, antihistamines, serine proteases, tissue plasminogen activators, structural deterioration of xeobitoics and carcinogens, and otherwise depletes detrimental factors. These factors are why developmental aged populations are resilient to particular viral vectors because embryonic plasticity foundations deteriorate xenobiotics.
Using two very large towels, drape the towels lengthwise across the head front to back and then from side to side, allowing the towels to drape down to back and chest and sides of arms. These cover eyes, nose, ears, and mouth to prevent entry of electromagnetic fields into orifices, the brain and through the upper respiratory tract to the lower respiratory areas. Folder a third very large towel into a thick fold of 6 inches wide, followed by wrapping the towel loosely around the neck underneath the towels draped over the head. Next use an extremely large hooded zipped jacket, placing this on the patient on top of all the towels. Pull the hood over the head and zip the jacket all the way up and closed. This should immediately protect the upper areas of anatomy, neck, and areas of soft tissue from allowing electromagnetic fields to enter and affect pulmonary and respiratory function. It may also be necessary to include EMF protection clothing or covering to add to the solution. It may also be necessary to wrap excretory orifices such as rectum and urethra by wrapping these areas in aluminum foil.
There is a requirement to find and close all internet sites. Secure firewalls on phones and computers. Change timezones on computers and phones. Changes locations in phone, computers and websites to very distant locations. Delete all social networks with specially attention to recently attached visitors, profiles, or susceptibility to physiological and behavioral changes resultant of people, people with large networks or people attaching to many similar locations, groups, social networks, as those of the patient. If these cannot be done, then disabling all protocols, all communications devices in phones or computers, placing these in air travel mode, and then turning these off, followed by wrapping these in aluminum foil, and removing these from the home or location where the patient is, may be necessary. Covering all power plugins and communications plugins, shielding all devices, televisions, computers and phones with quantum scalar EMF protection stickers, covering, faraday covering/netting, etc, as well as using EMF protection covering.
The research presented here presents a group of about 35 core factors, as well as additional group of expanded factors comprising about 50 or more, which are factors the lead to inhibition of PEMT or which are core factors inhibiting PEMT. Managing these factors beginning with the core factors and then managing the expanded group of 50 or more, provides a way to begin alleviating and preventing all disease.
However, it is important to understand why a civilization would knowingly withhold therapy that would have alleviated almost all disease and instead invented or discovered myriad new ways of inhibiting PEMT and increasing homocysteine. Each of these including wireless, electricity, withholding dimethylthetin, production of phthalates, C8, Teflon, imposition of abated being as a sanction that results in 550,000,000 detrimental outcomes and 1 million instances of abated being along with hundreds of millions of instances of abated being globally, not shielding all electrical infrastructure, choosing the most detrimental ways of obtaining water and not freely obtaining water from the atmosphere, choosing electricity production mechanisms that produce wasted, environmental detrimental, and human peril, all occur because the massively detrimental collateral and generational effect results in massive revenue from systems that are allowed to benefit from detrimental human outcomes. It’s a way of generating activity, business, activity and artificially increasing productivity statistics. The massively detrimental outcomes produce as a result are the true cause of almost all the geopolitical conflict, detrimental behavior and abated vital being experience since 1878. A best way to describe political activity since 1878 is to observe these as competitive interactions that ignore true causality, attributed causality for detrimental outcomes to humans whom have no awareness of these foundational factors that produce detrimental outcomes, and allow systems to escape being included as causal factors in a way that might allow detrimental outcomes to be prevented instead allowing detrimental human outcomes to occur and then turning humans upon eachother attributing causality to one another while the true causal factors are obfuscated and obscured.
The susceptibilities known as the 35 indicators and 50 or more expanded indicators, are essential susceptibilities which the universes have imputed into humans, allowing humans to sense changes in quantum, atomic, molecular, metabolic, environmental and universes levels systems and respond with changes to migration, behavior, preferences, activities, cognition and perception, as well as constructive activity. These susceptibilities are essentially because, otherwise, there would be no way of knowing when intangible detriment or impending detriment were emerging, potentiated or occurring. The observation that such susceptibilities are being allowed to persist, benefit is being obtained from detrimental outcomes which results, and the conditions which potentiate such susceptibilities becoming detrimental outcomes such as joblessness, homelessness, unassured nutrition, unassured clinical behavioral and medical care, not requiring care to acknowledge, alleviated and prevent empirical causality, and unassured outcome are integral factors.
Populations living pay period to period. Populations without stability and safety. All become susceptibility for harvesting to continuously fill places that managed detrimental behavioral and detrimental physiological outcomes.
Roemer’s axiom is a phenomenon in which construction of new healthcare facilities in an existing service area results in an increase in demand until the new facilities are filled at similar levels as the existing facilities in the service area. The phenomenon is confirmed by social constructs, Certificates of Need requirements for Hill Burton Act Provisions in which public funding for health services facilities requires a certificate of needs assessment . The certificate of needs requirements confirms that there is existing demand in the service area to prevent construction of new facilities in a way that would cause increased demand, increased instances of abated vital being and increase in detrimental outcomes. Massive hospital construction occurred outside of the Hill Burton Act provisions through private interests, resulting in a massive expansion in detrimental behavior, disease, epidemiological patterns, and consumerism. Consumer behavior is a known factor in susceptibilities introduced by homocysteine enabled subjectiveness, such that 90 percent of consumer behavior is known to occur from less than conscious interaction between physiology and systems. Pharmaceutical organizations utilize 50% or more of resources to advertise because homocysteine enabled subjectivity produces a competition between sources of advertising, marketing and sales, as well as cultural factors, bias, and disparities, a way that direct susceptibilities toward detrimental behavior, disease, mishaps, aging, victimization, or becoming a victim.
The Hill Burton Act was activated in 1946. Funding under the Hill Burton Act was discontinued in about 1998, in synchronization with the discovery and addition of choline to the list of require nutrients. Although the levels of choline recommended are grossly inadequate, such that scientific analysis suggests that between 4 and 7 micromoles per KG of anatomical mass are essential to human health.
The 35 and 50 or more factors are mostly applicable to the viral vectors and conditions involved in modern pandemics.
This information describes that disease and abated vital being occur because systems and populations are allowed to benefit from detrimental human outcomes and budgets, quotas, revenue objectives, margins, and objectives that in any way allow revenue, benefit or sustainment to be derived from any detrimental human outcome becomes causal to such outcome because no organization or system is able to prevent or abrogate such outcomes when it means that the organizational or system can no longer be sustained when such outcomes are prevented or alleviated.
Since 1878, all known humans exhibiting vital being no longer exist, specifically because dimethylthetin was withheld and the enzymes that process dimethylthetin were used to produce drugs that were provided to humans instead of providing them dimetylthetin or managing homocysteine in other ways. The resultant massive deterioration of social function and physiology resultant of omitting these priorities are responsible for massive detrimental behavior and massive instances of abated vital being. The use of abated vital being as sanction obfuscates these allowed exhibition of detrimental outcomes and causes more than 550,000,000 detriment outcomes and 1,000,000 instances of abated vital being each year, while also causing detrimental outcomes among systems workers, massive increases in travel incidents, decrease span of vital being, and causing similar increases of detrimental outcomes among global populations. The inflated cost structures involved in these contrived nuances of human detriment include choosing massively more detrimental and expensive ways of obtaining water and obtaining electricity which can be obtained freely using ‘free water from atmosphere and using permanent magnet solutions’ such as calnetix which produces such massively more efficient generation of free and wasteless electricity. These describe a remarkable focus on obtaining massive levels of revenue by allowing and causing disease and detrimental behavior as well as choosing the most toxic and detrimental ways of producing electricity and managing water. In each instance, these analysis present that disease should not exist anymore, homelessness should not exist, water should be freely available with simplicity and no detriment to environment, electricity should be free and with no detriment to environment, and detrimental behavior should be almost nonexistent., such that these only continue to occur because it generates massive levels revenue and is required when a civilization does not freely assure the factors that comprise the human, social, behavioral, physiological and economic condition.
The data clearly observes that the integration of Hydride into phospholipids in membranes by PEMT or constitutive integration of Choline or phosphatidylcholine, transforms cellular environments into biologically active environments because this integrates hydride within CH3 or methyl groups into physiology. This integration of hydride produces a capacitant field that is accompanied by a negative polarity that attenuates into the background environment outside of the mitochondria through the activity of PEMT2 and outside of the endoplasmic reticulum enabled by PEMT1, that is also accompanied by enhanced exhibition of ether linked antiinflammatory fatty acyl moieties, resulting in enhanced insulation that is increased some by PEMT1 and increased even more specifically by PEMT2. This context enables foreground of H+ to contrast a background of net -, culminated in a gradient that enables redox potential. This redox potential is intracellular, extends to the extracellular environment, enables NAD+/NADH, NADP/NADPH and other redox factors such as FAD/FADHM, FMO and other factors to exchange Hydride or exchange redox factors. Oxidative Phosphorylation or cellular respiration known as the electron transport, all to occur, enabling clean energy or current to be used for activity along this gradient or be utilized for activity that occurs in opposite direction of gradients.
This capacitance at tissue levels in neurology, produces a field within tissues and neurological tissues, that constitutive conscious cognitive function.
The literature now clearly presents that the function of PEMT as a percentage of activity in any cellular entity and among tissues, as well as among physiology, is directly correlated inversely with disease, level of disease, impairment, level of impairment, exhibition of abated vital being, impaired consciousness or being less than conscious, detrimental behavior, susceptibility to detrimental behavior, deterioration of areas of neurological centers required for social function, impaired rewards systems function, deteriorated conditioning, impaired conditioning recall, deteriorated memory, and separation of behavioral control from the control of environmental or locational behavioral queues/stimuli/response pairings, dementia, impaired ability to learn, impaired spontaneous regeneration of anatomy after injury, and all nuances of conditions linked to aging.
PEMT is important because it is know being confirmed that PEMT2 function in the mitochondria is enabled because all mitochondria, hundreds in one cellular entity, and even ones that move between cellular entities within axonal regions and sarcolemma to other cellular entities, are attached to Endoplasmic Reticulum through a region known as the mitochondrial associated membrane. This membrane is connected through channels that are enabled by Mfn1 and Mfn2 enzymes that participate ubiquitylation, Autophagy, and Mitophagy which recycles organelles and mitochondria. This membrane is how the Endoplasmic Reticulum shuttles Phosphatidylserine for Phosphatidylethanolamine synthesis, phosphatidylethanolamine, and Ca2+ into the mitochondria. The literature is even now suggesting that PEMT2 activity occurs in the mitochondrial associated membrane instead of occurring in the other membranes of the mitochondria, but this is being confirmed at this instance by more specific studies. This explains why in oncology, disease and detrimental behavior, as well as aging, PEMT2 activity is obliterated and PEMT function generally is observed to be impaired in studies.
Homocysteine increases when PEMT is inhibited or when methyltransferases that manage toxicity, xenobiotics or other toxic conditions or factors perform methylation of these potentially detrimental factors. Homocysteine inhibits PEMT transactivation which causes P53 expression, causes PTEN expression to protect P53 from ubiquitylation by MDM2, while PINK1 is activated by PTEN. PINK1 moves to the outer membrane of mitochondria that has impaired polarity/capacitance, and moves to the inner membrane of mitochondria which have adequate capacitance/polarity, such that PINK1 in the outer membrane of mitochondria recruits Parkin to the outer membrane causing PINK1 to be processed and beginning the process of mitophagy or recycling of the mitochondria.
However, when the Mfn1/Mfn2 enabled exchange of phosphatidylserine/phosphatidylethanolamine and Ca2+, as well as exhibition of Phosphatidylinositol on locations of membranes at which emerging autophagomes emerge, are individually or all diminished, apoptosis pathways that emerge from mitochondrial activation pathways become impaired, resulting in much of the conditions known as oncology.
The exhibition of mitophagy can be enabled by phospholipase D expression, which prevents Macroautophagy and specifically enables mitophagy in a way that prevents impaired mitochondria from sending out signals to cause an impaired cellular entity to deteriorate itself to prevent progression of disease.
Phospholipase D is important in this context because Macroautophagy is impaired in cellular entities exhibiting oncology and many disease, such that these impaired cellular entities rely upon proteolysis to rapidly recycle intracellular enzymes and metabolites in a way that makes the recycled material availability of diseases, disease pathways, pathogens or pathogenic circumstances. Inhibition of Proteolyse by 20S proteosome inhibitors cause pervasive cellular entities exhibiting oncology to deteriorate. Those which do not exhibit oncology and do not exhibit disease can sustain themselves using Macroautophagy, but phospholipase D can divert Macroautophagy to Mitophagy, preventing impaired mitochondria from activating apoptosis and deterioration pathways by causing impaired mitochondria to become recycled before they can efficiently or stably introduce apoptosis pathways.
Inhibited transactivation of P53 results in upregulation of choline kinase which adds atp to free choline to produce phosphocholine which acts as substrate for proteolysis and provides ATP for proteolysis that sustains oncology because Proteolysis requires ATP and because hydride is been translated to ATP or ATP has been integrated into Pyruvate to produce aerobic glycolysis that occurs when pyruvate and ATP flourish unregulated by P53 suppressive mechanisms that are invoked when PEMT is inhibited. ATP and Pyruvate flourishing in this regard is dirty energy and attenuates into all manner of pathways not possible when the energy is Hydride, reliant upon hydridic influence or regulated in a PEMT enriched environment.
Inadequate substrate for PEMT inhibits PEMT catalytic activity and this can be linked to upregulation of AP1 or SP1 which increases CDP Ethanolamine pathway but inhibits PEMT and directs substrate and products of the CDP Ethanolamine pathway to the CDP Choline pathway as well as to proteolysis.
inhibition of PEMT transactivation results in upregulation of choline kinase which increases production of phosphocholine. Inhibited activity of PEMT but which occurs when PEMT has been produced through transcriptional transactivation, results in upregulation of AP1, SP1 and upregulation of the CDP Choline pathway that results in upregulated production of phosphatidylcholine that does not have focused benefits provided by PEMT1, PEMT2 or PEMT3. This phosphatidylcholine from the CDP – Choline pathway can be directed toward phosphatidylserine then to phosphatidylethanolamine to activate PEMT activity. However, when PEMT is inhibited, phosphatidylethanolamine can accumulate although it can also be depleted by pathogenic depletion otherwise causing sustained directing of phosphatidylserine to phosphatidylethanolamine. Phosphatidylethanolamine accumulation inhibits phosphatidylcholine direction toward phosphatidylserine and phosphatidylserine to phosphatidylethanolamine, enabled enhanced production of ceramide by nSMase/aSMase, although ceramide enhances the potential for cellular deterioration and apoptosis while it also produces phosphocholine, thereby supplying substrate and energy to proteolysis which sustains oncology.
Phosphocholine is a general, opportunistic energy molecule used by pervasive disease and pervasive oncology, as well as pervasive pathogens, often merely because its deterioration by proteolysis frees ATP and sustains cellular membrane through freeing phosphatidates, and often merely because phosphocholine can be used directly by pathogens and provides phosphate groups for phosphorylation pathways that comprise the crux of survival signaling that occurs to prevent cellular entities from exhibiting apoptosis when all other ways of survival are inadequate during a particular challenge, event, context or condition.
However, choline kinase, when upregulated, diminishes the affect of CHOP which promotes apoptosis, and choline kinase enhances the unfolded protein response which is a change the endoplasmic reticulum activity and focus, as well as causing changes to sequestrome and ubiquitylation pathways in order to find proteins impaired from endoplasmic reticulum dysfunction, repairing, removing or recycling these proteins and enzymes to prevent apoptosis or cellular deterioration otherwise. Choline kinase production of phosphocholine can typically be directed toward upregulated proteolysis during oncology and disease but can can also be directed through subsequent factors of the CDP choline pathway toward phosphatidylcholine production, even possibly joining substrate from the CDP Ethanolamine pathway that is directed toward the CDP – Choline pathway because PEMT function is impaired to prevent depletion of phosphatidylethanolamine culmination of the CDP – ethanolamine pathway, resulting in accumulated Phosphatidylethanolamine. It should be mentioned by CEPT1 or the enzyme that performs the concluding phase of the CDP – Ethanolamine pathway, specifically selects or produces substrate and produces enriched with ether linked, DHA, Oleoylate, Palmitoylate first fatty acid in beta oxidation, extended arachidonate, insulated antinflammatory, capacitance enhancing fatty acids, but also utilizes a small amount of its catalytic activity to produce phosphatidycholine, mimic both the CDP – Choline pathway and PEMT activity in producing phosphatidylcholine.
Ceramide, however, can be directed through Sphingosine Kinase toward S1P and S1P activates inflammation and survival signaling through G Proteins, GTPase, ATPase and S1P receptors, as well as invokes Hydrogenase/Dehydrogenase PDK1 activity that prevents Pyruvate from being directed toward acetyl – CoA and acetyl-choline storage through the activity of choline acetyltransferase while this also enhances the directing of pyruvate to PARP/PARS signaling occurring millions of times each day in each cellular entity to deplete NAD+ that is produced when NADH and pyruvate are processed by Lactate dehydrogenase to produce NAD+ and Lactate anion. NAD+ is required because P53 and NAD+ depletion, enabled by PEMT inhibition and P53 activity, inhibits the pentose phosphate pathway where nucleotides used in DNA Repair/replication are produced, such that PARP signaling occurs persistently, depleting NAD+, until enough nucleotides are available to repair/replicate DNA, while remnants of NAD+ depletion are processed by nicotinamide methyltransferases that enhance s adenosyl homocysteine levels when these methylate nicotinamide remnants in a process that causes already differentiated cellular entities to exhibit apoptosis and which cause newly produced cellular entities and stem cellular entities to gradually lose the ability to experience apoptosis, obviously being canonical conditions for oncology.
This explains what can happen with acetylcholine storage being diminished, resulting in increased free choline and upregulated choline kinase activity as it attaches ATP to free choline resulting in phosphocholine. However, S1P represents climatic event in survival signaling because it activates diverse inflammatory pathways and because when it is depleted by S1P Lyase, the diminished availability of S1P can be incomplete and S1P Lyase, although providing phosphoethanolamine hexadenal for DHA synthesis, also is an escape pathway used oncology and diseases to produce resistance to therapies.
Also, S1P Lyase enhances the activity of GSK3, and GSK3 emerges as a pivotal factor in pervasive differentiation pathways which has to be exhibited in a tightly regulated, PEMT enriched and sometimes gluconeogenic/Hydride pure environment to prevent being commandeered for disease. When analyzing pervasive molecular, protein and autophagy, and differentiations that were required in detrimental nuances of aging, disease and detrimental behavior, unregulated GSK3 was essential, causal, and often constituting the culminating factor for progeritin and other diverse factors required in the detrimental nuances of aging. GSK3 inhibits the enzyme that lyses or frees glycogen from amyloid fibriles which store glucose and is important factor in obesity, disease and particular differentiation pathways but perform as a top level regulator of diverse micro level differentiation pathways such Wnt, B Catenin, Catenin and many, many others. GSK3 has a tail that use to activate other factors but this tail can be obscured by GSK3 itself, and GSK3 integrates with P53 in a way that is essential to particular changed behavior by GSK3 ad P53.
Thus, there emerged a very reasonable perspective of the big picture items presented here. Homocysteine inhibits PEMT and PEMT increases Homocysteine. Homocysteine inhibits PEMT and PEMT inhibition as well as methyltransferase activity that performs methylation increases homocysteine. Homocysteine increases Bax, while the Bax promotes a cellular entity to experience apoptosis and Bcl2 prevents apoptosis. Disease in which cellular entities accumulate without experience apoptosis or exhibit resistance, involve upregulated Bax compared to Bcl2. Disease the result in cellular entities experiencing too rapid deterioration, involve upregulated Bcl2 compared Bax. Bag3 is linked to proteolysis and upregulated Bcl2 while Bag1 is linked to Bcl2 enhancement compared to Bax as well as is not linked to Proteolysis but, instead, versions of autophagy. Bag1,2,3,4,5,6 however are all Bcl2 linked proteins that affect Bax to Bcl2 ratio.
Conditions that involve differentiation impairment, even ameliorated aspects of aging, typically involve GSK3, such as those factors observed with aging.
However, it is the inhibition of PEMT that is integral in this conditions and the impairment of macroautophagy such that mitophagy occurs instead macroautophagy or other autophagy, as well as impairment of the endoplasmic reticulum transfer of Ca2+, phosphatidylserine, and phosphatylethanolamine to the mitochondria which are pivotal events in these contexts. These describe why and how the protective mechanisms of PEMT1, PEMT2 and PEMT3, particular PEMT2, are diminished, impaired, and even obliterated in disease. These factors were found to be pivotal causes of every nuances of aging included in the analysis and could even explain why particular less than optimal conditions result in improved span of being in organisms.
Importantly, a pivotal observation was that StARD7 which is protein that exhibits moieties that attaches to phosphatidylcholine and cholesterol, thereby being integrated into START Proteins of phosphatidylcholine in diverse membranes of cellular entities, encapsulates cholesterol into its protective pocket and enables transport of cholesterol to the Mitochondrial outer membrane where it is processed by PARL protein such that mature START domains with negatively polarized amino acid moieties are directed into the mitochondrial intramembrane space and while less than mature START Domain exhibiting proteins are directed into the cytosol. PARL can also process PINK1, PARK processing of StARD7 is required for mitophagy, and StARD7 is required for optimal and typical Mitochondrial function. The shielded transfer of cholesterol by StARD27 within START Domains, or within the Start domains of star proteins, is essential to optimal health and can even assist in performing rescue of impaired mitochondria.
The cholesterol is processed by Cytochrome P450 scc to Pregnenolone, an inhibitor of Choline Kinase, resulting pregnenolone becoming translated into Androstenediones, Testosterone, Estradiol, Estriol, Estetrol, Estestrone, and other glucocorticosteriods and hormones linked to male and female physiological structure and function. Estradiol evenly activates estrogen receptor alpha and beta, while estrone upregulates estrogen receptor alpha compared to beta, such that estradiol and estrone both occupy the perfect 13 sequence estrogen receptor response element activation sequence, which also occurs in the promoter region for PEMT. Thus, Estrogen receptor alpha, activated, causes transcription of PEMT while estrogen receptor beta causes expression of PEMT in a way that regulates or diminishes estrogen receptor alpha transactivation, while estrogen receptor alpha upregulates AP1 and while estrogen receptor beta downregualtes AP1, followed by AP1 inhibiting the activity of PEMT generally, constituting autoregulatory system in which PEMT expression is inherently self regulated by PEMT when estrogen receptor alpha enables PEMT Expression along with the introduction of estrogen receptor alpha which regulates estrogen receptor alpha using different mechanisms and indicators, along with inhibition of AP1 allow the diminished levels of PEMT expressed by estrogen receptor alpha when diminished by estrogen receptor beta to become more fully catalyticaly utilized.
Thus, to conclude, the analysis linked to the information presented here, presented these factors as the systemic and systematic factors that cause 99.5 percent of disease, detrimental nuances of aging and detrimental behavior. Because these are known. what is know of now as aging, should not be occurring. Genetic disease requires these mechanisms pervasively and genetic disease can be eradicated using CRISPR gene editing. The early results in gene editing have been limited because of complexiity in assuring that all cellular enities recieve the editing payload, while, curiously, protein transduction domains have been available since the 1990s that allow CRISPR gene editing payload to be introduced in every cellular entity of physiology with the efficiency of a water molecule. It is curious or even telling why transduction therapy has not been utilized in this regard.
Regardless the amehsi specification has been published now in some reputable internet venues and the new website under a new name, publishes the details presented here. Although the websites new address has been purposely obscured by numerous new websites that direct a web search with the full .com name to many pages of other websites unless the search is conducted with the website name in parenthesis, it is presented here that that new model for health is wellness and individuals, groups, and communities should begin to understand these mechanisms and utilize the new research website to begin a different manner of being that is without disease, detrimental health status and unnecessary detrimental outcomes. The industry that are easy to impugn in this regard have been integral to the production of this new model of wellness and unlimited potential for vital being.
It is hoped that humanity is able to realize this potential with all due immediacy.
These are very important because a review of the cause of Sarcoidosis clearly observes that atmospheric pollution, dander, allergens, animal dander, mold, microbes, and other factors enhance inhibition of PEMT and the allergic response that produces homocysteine. Similarly, C7/Teflon/perfluorooctanoic acid, entered awareness through many decades of analysis, and it was found to cause increase in a number of inflammatory mechanisms presented here as inhibitors of PEMT and upregulators of Homocysteine. Perfluorooctanoic acid, for instance, was found to upregulate pulmonary macrophages which are primary causes of granulomas by 2,400 percent in one study. This toxic factor is found in pervasive consumer products. Another study and cinematographic production observed that perfluorooctanoic acid has been allowed into the environment and has contaminated more than 99 percent of the organisms on earth in at least some level. A Similar analysis observes that since 1878 when dimethylacetothetin was discovered and enabled management of homocysteine, toxins, causes of oncology, atmospheric pollution, communications/electrical fields have been introduced that have become the principal causal factors to pervasive disease regardless of consideration of dimethylacetothetin.
The popular literature has again started to produce propaganda promoting that diseases are somehow natural and immitigable, while vital being, also, by such entities, is presented as being wanton, expendable, limited immitigably. Ignore those entities, ignore those assertions, and utilize the information here relegate that nonsense to aspects of the human experience which become increasingly eradicated from the ability to affect human populations.
Also important. The very systems that are being presented in the existing sociopolitical climate as being detrimental were integral if not already having produced the information utilized in these analysis. These systems started eluting information specifically used in these analysis as early as 1900 and in the decades which followed with progressively increasing specificity. Often, the more detrimental, and publicly presented an outcome may be, the more precise and more pivotally enabling the information linked to that outcome has been.
Obviously, if alarm bells go off for more than a century without acknowledgment of causality or resolution of causality, eventually the alarm bells themselves will begin to become problematic and all manner of unintended outcomes are potentiated.
It suddenly becomes clear why autocracies emerged in the world before formal democracies emerged. Democracies require technological innovation, because without such innovation, democracies as they now may be, risk enabling the abrogation of species.
Why? Two examples are clear. The discoverer of how to obtain plasma for storage and utilization, was excluded from utilizing the capability in particular settings, excluding from a principal national role in implementing such capability and even incurred abated vital being from not being able to fully utilize such capability when the discoverer required such capability. Similarly, a leader of a civilization, recently to this composition, with the namesake of the research journal in which an 1878 article presents how to use dimethylacetothetin to deplete homocysteine, was deprived of that capability at an advanced age. Dimethylaceothetin would have likely added many more decades or centuries to the duration of the vital being for such a leader. These events occurred among the most advanced Democracies. The conclusions are that Democracies was be continuously trained to prioritize Life. Imperfect Democracies have a propensity to be Majoritarian and thus find nuances of the population who can be excluded and attributed causality for all of the detrimental outcomes that are required for the status quo to persist. Democracies, however, do not have to be this way.
However, in an Autocracy, one thing is clear. At least 1 person, 1 group or an Aristocracy, is sure to be prioritized, compared to the deprioritization of all Humans that can occur in democracies. A democracy early in Human experience in which biomedical capabilities are excluded from being utilized even for leaders and an aristocracy, would have resulted in abrogation of species. Autocracies were might have been essential to the continuation of the Human experience in these early junctures, although it is clearly not suggested here that an autocracy is optimal in all manner of administration of the affairs of civilization and that autocracies have led to and even provisioned their own democracies in acknowledgement that Republics are optimally guided by the populations which comprise them.
However, this presumes that the population guiding a Republic are informed and are able to discern opinion from truth, presuming that such truth is linked directly to empirical nuances of reason. Thus, while it is true that abated vital being occurs among populations, the empirical nuances of reason implore that humans functionally, if not cognitively, have an inherent priority in resisting the occurrence of such observed outcomes. Although it seems plainly obvious that such priorities as Life, Liberty and Pursuit of Happiness exist in civilizations, outcomes clearly present that abated vital being is acculturated. Thus, when does such acculturation constitute assistance and even causality, compared to mere observation? Not managing PEMT pathways as priorities seem to constitute such assistance and seem to constitute causality.
Although these analysis seem like hyperbole, such analysis are important in the existing sociopolitical contexts. There is a substantial risk that systems have emerged as being incapable of being attributed causality for pervasive Human outcomes that do not occur unless systems are exhibited. Thus, when detrimental outcomes occur, systems implement interventions that do not acknowledge the empirical causal factors, attributing causality of these to humans and ignoring the 12, 20 or 50 factors that have to be exhibited for detrimental outcomes to occur, including the factors that constitute deterioration of metabolic, molecular, physiological, perceptive and cognitive bases for social behavior. Pervasively, these nuances of physics, biology, and biology, are excluded from deliberations regarding outcomes, structure of sanctions, and even are excluded from priorities in care, resulting in cascading Human events that result an endless supply of detrimental Human outcomes.
Thus, systems, implementing interventions, expose their workers to an endless supply of detrimental outcomes, associates, conditions that confirm biases, and scapegoating, while not managing these 12, 20 or 50 factors even for systems workers themselves. The result is, that true, incipient, causal factors, and activating mechanisms that cause detrimental outcomes among populations and workers within systems alike, are omitted from ascertainment, acknowledgement and alleviation. Additionally, when facilities managing detrimental Human become inadequately supplied with unfortunate outcomes and Humans to attribute such causalities to, systems workers then become substrate for the sustainment of systems.
A most detrimental potentiality is that systems can implement social constructs and sanctions that are grossly inadequate, caused increased detrimental outcomes, producing generational and collateral detriment, then benefit from doing so. Similarly, by attributing causality of detrimental outcomes that occur as a result of less than empirical resolution of causal factors in such regard, then system workers can be scapegoated. Thus, systems can escape from having to acknowledge and improve the ways in which systems cause detrimental outcomes, escape inadequate training, produce grossly obfuscating concepts such as the presumption that ‘a lot of training is equal to effective or adequate training’, as well as sustain an unwillingness to acknowledge the 12, 20 and 50 factors which would pervasively alleviate or prevent detrimental outcomes. These context exhibit populations being divided and turned upon one another, somewhat assuring that cognitive permeation of the subterfuge might not ever occur. It’s a canonical silencing of the lambs and silencing of the doves, resulting in synthesis of new mechanisms for Humans to impart detriment to one another using systems without having to understanding or acknowledge any of the causal factors. Likewise, systems, in this way, no longer have to responsibly ascertain the suitability of workers for the roles in which they are place, merely scapegoating such workers when less than optimal outcomes occur.
If every human, in what is the most wealthy economy ever to have existed, has a salary that assures adequate sustainment of social, human, behavioral and physiological requirements, then, would there be a reason to have such intricate nuances of social constructs and sanctions? Were the framer’s of the Constitution intending to assure specific assurances that maintaining of detrimental artifacts specifically produced to cause detriment other humans even when these have become among the most detrimental vectors to Life, Liberty and Pursuit of Happiness? Particular nuances of the existing sociopolitical context exist in substantial dissociation from the incipient nuances of reason, the favor of the Universe and even the intended presumptive foundational assurances of Life, Liberty and Pursuit of Happiness. Humans cannot responsibly dispense with control over Human Life, except in absolute assurance thereof. Outcomes otherwise, merely demonstrate inadequate capacity. Thus, if one becomes aware of inadequate perspectives or biases, how effective are systems are in enabling these to be acknowledged, managed or alleviated in their workers. Similarly, how effective is a civilization in assuring that people coming to understand such inadequacy might be sustained in satisfying social, Human, behavioral and physiological requirements.
How many people, for instance, participate in systems that have less than optimal influence or which they are not able to impose their own priority of Life, Liberty and Pursuit of Happiness when it exceeds that assured by such a system, whom are empowered to do so? How many people producing, exporting, importing and distributing artifacts specifically produced to cause detriment to others might do otherwise if other opportunity or an assured reasonable stability achieving income were assured?
Thus, all that is required is an absolute priority of systems or a lack of absolute priority for Human Life, Liberty and Pursuit of Happiness. Outcomes, then, can become considered only in their most proximate nuances of time, causality, context, circumstance and outcomes, ignoring all of the factors that were required to be their disjointly to these proximate nuances, in order for systems to be directed toward scapegoating virtually any nuance of the population which a majoritarian influence decides to utilize in such regard.
Thus, a democracy, unless informed with understanding, acknowledgement and priority of considering the bases of biology, physiology, perception, cognition, behavior and how systems affect these, has a propensity to potentiate abrogation of species. It is perhaps institutions that readily present mercy and forgiveness, which are nuances of the truth that is causality that is 99 percent extrinsic to humans, along with those institutions of art, science and humanities that have invested in and present understanding of the arts, sciences, humanities, applied research and other essential capabilities, which prevent a Republic and a Democracy from abrogating itself and possibly causing abatement of the Human experience. Certainly, a Democracy in distant ancient eras would have been dominated by inadequate understanding, resulting in potential for such civilizations to become abated. Somewhat inclusively, this very outcome has occurred among ancient civilizations.
These dynamics explore, more intricately, the observed inherent propensity for any system of the Universe to prioritize itself over its incipient circumstance, incipient purpose, utility and over Humanity. Such that empirical resolution of detrimental outcomes, along with prevention, alleviation and acknowledgement of empirical and incipient causalities can become secondary to sustaining the system, often by not implementing empirical resolution to detrimental outcomes in a way the absolutely prioritizes Humanity. Attributing causality to humans for detrimental outcomes in this regard, seems to be a way for systems to merely persist, preserve and perpetuate the status quo. A social construct and a sanction, as well as an Axiom in contexts of research, all represent an artifact utilized to replace empirical understanding. Bias also seems to perform in similar capacity.
A practical example is a building’s hallway leading outside through a set of Doors, being exhibited in a populous path of exist from the building. Detrimental outcomes are presented as someone or something causing people leaving or entering the building to stumble, fall or even fall into one another. The status quo exhibits that people falling to the ground and people falling into one another attributed causality for such outcomes. The cause of the falling is not ever acknowledged in deliberations, care, sanctions or outcomes. Thus, when facilities benefiting economically, social, culturally, through quotas, occupancy levels, or in other ways become empty, the factors causing such falling can be increase directly by observing more doorways or can be increased indirectly through systems of mechanistic links, such as decreasing the price of meat, chicken, eggs or fish, and such as increase electricity or atmospheric particulate, and even by constructing more hospitals and facilities use to manage such outcomes, all can be implemented.
Particularly, in some systems, there are specific exculpatory provisions preventing the bases of biology, behavior, and physics from being utilized to explain what is happening, causing Humanity to be turned upon itself, mitigating immunity in systems that is one of the only context in which these factors are being acknowledged, thus reducing Human outcomes to the lowest common denominator of impaired assurance of Life, Liberty and Pursuit of Happiness.
The gating mechanisms are the inherent nature of systems, as well as the absence of an assured salary and level of sustenance in civilizations, because this produces a circumstance in which Humans in any organization and systems rely upon the outcomes intervened by, managed by or otherwise causing utilization of the services, products or factors produced by such system or organization. This is known as Roemer’s axiom, such that is it well known that building new Hospitals in a service area results in increase of detrimental outcomes until the new services are utilized at nearly the same level as was exhibited when only the first Hospital was exhibited. Thus, when global resources are used to produce health and wellness capabilities, then imported into civilizations founded upon presumptions of assured Life, Liberty and Pursuit of Happiness, the result is that the inherent ability of Humans to derive sustenance from the biome and the Universes becomes directed at deriving revenue from the utilization of those products and services. The 5 to 10 million instances of detrimental artifacts using projectiles that are imported into such a civilization along with the production of such artifacts in such a civilization, including the pathways of distributing these, transforms the Universes, the biome and civilizations to exhibit those outcomes that require the utilization, purchase or obtainment of such factors.
Pervasively, there seems to be an unwillingness to read the small amount of research required to demonstrate these linkages conclusively. Roemer’s axiom has long been refuted then acquiesced to by researchers and analysts who gradually able to perceive these dynamic in all manner of systems and outcomes. The abated use of Hill – Burton Act Provisions for Certificates of Need regarding health resources along with the repeal of the executive order preventing usage of abated vital being as a sanction, each have tight synchronization to emergence of pandemic microbial vectors across civilization, which is the context in which abated vital being is decreased when Hill – Burton Provisions and moratoriums preventing usage of abated vital being as a sanction are in place.
Thus, the continued ignoring of PEMT pathways in care in behavior, as well as the imposition of abated vital being as a sanction, along with overt exclusion of Roemer’s dynamics from being integrally included as mechanism of control for how systems affect population health and behavior, all have emerged as the most detrimental vectors to Human populations and stability of civilizations. These have become of potential despeciating potential, as the expanding influence of Humans to the universe through systems of civilization, instead of the only through the Unique interaction capabilities of human physiology and behavior, began to inform the Universes how civilizations and thus the species, prioritizes itself or prioritizes Humanity. Heretofore, the Universes inclusively know and acknowledge, through the favor afforded Humanity in its physiological and cognitive abilities, Humans as the culmination of the creative forces of the Universe.
These present very clearly why Majoritarian Democracies within Republics could only be sustained in modernity. Eras before modernity exhibited substantial potential for abrogation of species since withholding only a few innovations in research, understanding and health in earlier eras may been a determinant in the sustainment of civilizations and sustainment of species. The current era exhibits that particular nuances of populations are scapegoated, exculpating consideration of the bases of physics, biology, and behavior. The current era exhibits the highest numbers of species which are becoming extinct. The potential outcome is that the Universes being informed of a depriotization of Humanity might become integrated with the reality that Humans really are a minority among the Biome and the Universes, causing the kinds of realigning elections that hardly any social or political context seems to be able to adequately perceive.
The obvious conclusion here is that producing localized nuances of reason, dissociated from Human priorities, it is possible to produce an endless supply of detrimental outcomes that seem be reasonable using only the means as a way of analyzing the outcomes produced. Exclusion of PEMT pathways from care seems reasonable, because it enables sustained, recidivism in emergency care, disease and detrimental behavior that results increase revenue higher case mix ratio from higher DRG scores. Executives and providers who focus on PEMT exhibit lower recidivism and decreased revenue for fee for service revenue/payment schemes, risking replacement for those less aware or less willing to provide care at this level. Similarly, outcomes in which abated vital being occur are explained away with statistics, and are dissociated from presumptive priority of Life, Liberty and Pursuit of Happiness.
There can be to be enough opportunity with adequate pay civilization to focus on assuring optimal Human outcomes at physiological and behavioral levels without allowing any entity to obtain benefit, merit, revenue or profit resultant of detrimental Human outcomes or requiring detrimental Human outcomes.
Hello.
It would be difficult for any practicing provider to provide the information here, in a professional capacity or otherwise. It is not presented here if this researcher is a practicing provider. The answer make not make anyone reading this particularly comfortable. However, I was educated at a university with a large teach hospital, specialty care and primary care graduate medical education institution. Researcher learned this pathways on an information technology teams with a diverse group of health industry worker where credentialed in diverse nuances of clinical, primary, specialty, mechanical and molecular levels of therapy and care. 2 1/4 decades of tracking molecular pathways in this regard. Researcher has graduate, undergraduate and certificate education credential in arts, science, technology, and in industry level data, analytics and administration.
Also, the researcher has participate in care processes. One such instance included performing as care liaison to manage interaction between a care subject and practicing clinician for disease involving atypical proliferation of cellular entities. Forgive the euphemism. The practicing physician was open, communicated freely what their analysis was and what therapies were being used for what reasons. Interactively, the practicing physician and researcher were able to ascertain that every version of disease of atypical cellular proliferation, typically known by another commonly used name that most are familiar with, required both the inhibition of PEMT and upregulation of Choline Kinase. Thus, the adjuvant therapies being selected, inhibitors of Aromatase and inhibitors of Estrogen Receptors, each would enhance the cause of the disease. The aromatase therapy was decreased to 1/4 of what was already being prescribed.
Subsequently, the research and the practicing physician were able to ascertain that the calficiation deposits observed in the condition were the result of pH levels being impaired in the microenvironment, used of antacids that were providing Calcium Carbonate, resultant of Oxalate deposits resultant of Hyperoxularia linked to diabetic pathology, and each were exacerbated by electrical signals being presented by Cardiac Pacemaker implanted in the tissue where the condition originated.
Additional analyses revealed that not only was Cardiac Pacemakers producing electrical fields, but the environment was inundated with wireless communications, uncovered electrical outlets, mobile communications devices, and appliances. The industrial, clinical and health and safety information clearly presented inducible nitric oxide synthase as an inhibitor of PEMT caused by these diverse fields along with energy being emitted by the pacemaker. Also the ponderomotive effect was found to cause asymmetric flow in vascular areas that results in deposits along the vascular wall, resultant of electrical and magnetic fields. Thus, iNOS was depleting intracellular calcium, poking holes to deplete endoplasmic reticulum and extracellular Ca2+/L – Arginine, as well as causing collapses of the sarcolemma, amoeba shape of cellular entities, impaired metalloproteinase activity, deterioration of the extracellular matrix, depletion of myelin basic protein that requires L-arginine, sequestering away L-arginine and Ca2+ away from eNOS and nNOS, as well as causing systemic gradients in Ca2+ being depleted from bones because of such strong iNOS signaling. These factors also potentiate intermittent infarct activity as uncoupling of any of the NOS enzymes, including vascular pathology from eNOS impairment, vascular pathology from deposits along the soft tissues and among vascular pathways, calcification from detrimentally enhanced calcium in circulation, intermittent dementia from uncoupling of eNOS/nNOS, and exacerbation of diabetic pathology as energy fields enhanced renal iNOS and impaired renal eNOS/nNOS.
Energy protection dots were placed on the windows of the home near electricity and communications wiring, in the direction were electricity tranformers and electricity substations were located. Also, electricity plugins or power outlets were covered with duct tape and a energy depletion capability for the bed was devised that also included a grounding wire suspended over the bed, both of which were then linked by a wire to a long metal artifact that was extended into the ground.
Care activities were then expanded to the primary care physician whom was equally open and capable, although there was already being implemented ways of managing PEMT pathways at this level.
After reconstituting the PEMT pathway including Choline, Phosphatidylcholine, Trimethylglycine, Folate, S – Methylmethionine, Glutathione, cystathione, Vitamin Supplement and mineral supplement, the multiple times per month visit to the Emergency Departments no longer occurred, the patient improved from immoble to being able standup up and walk with support, see over long distances and exhibit spontaneous recall along with spontaneous expression of specific tastes, asking for specific foods, and conversion that included required analysis, thinking, and memorizing cognitive concepts for extended duration. B12, B6 were also specifically included. Superoxide Dismutase, L-arginine, Catalase, and N Acetyl L Cysteine, all were included. Berberine and Curcumin were also included.
Kidney stuff was then utilized to help stabilize Hyperoxaluria, Bottled water was already being utilized to avoid Chlorine/fluorine and particulate, which are also sources of iNOS.
The specialty care health provider then, after several follow up instances, completely removed the inhibitor of estrogen, with the requirement that complete supplemental regiment be continued, sources of Carbonate in therapies, antacids and foods were to be kept to a minimum and vitamin K2 be utilized to prevent calcification of soft tissue by managing the increased Ca2+ levels resultant of iNOS activity.
Over the long term for the nonagenarian, more than 90 years old, the only time an opportunistic microbial condition occurred and every instance in which a visit for emergency care occurred was after a week or more lapse in implementing the regimen along with exposure to energy fields outside of the protective fortress built to manage detrimental influences.
This model, clearly presents that a role is required for each patient in which assuring of these foundational pathways occurs interactively with specialty care and primary care. During the complete duration of improvement, the care subject did not every fully receive the recommended dosages for the supplements because of social, cultural and logistical issues which cannot be elaborated upon in this context.
These suggest that modern medicine seems to be inadequate only because it requires that the foundational nuances of metabolism, biology and physiology be mapped, assured and analyzed to find gaps in therapy as well as inadequacies in physiology.
Choline was already being supplemented in small amounts requiring less reliance upon insulin injections and more stable conditions, but the choline supplement include Calcium carbonate and other factors that were actually included in the deposits linked to exhibition of atypically cellular proliferation. Choline supplementation and Kidney Stuff stabilized the disease and regressed the level of Kidney pathology.
Although the status quo for the care subject could be indefinitely sustained in this context, assurance of the recommended dosages would caused regression to independent function for the care subject.
The omitting of visits to the Emergence Department, however, revealed gaps in care continuum because physical therapy, nutritional support, skilled in home care, occupational therapy and physical therapy, all were only linked to episodic visits to the emergency department. Thus, it was clear that care systems like other systems were having a difficult time integrating these capabilities and this N – Tiered full stack application of their resources unless being galvanized by an Emergency Room visit and admittance for inpatient care.
The opportunities for care continuums to be independent of if care and continuums emerge from or are conducted in inpatient, outpatient, office visit or home setting is imperative in this instance. While, also, an independent, objective, clinical role that manages care in all of these settings by setting and assuring a foundational basis for biology, physiology, metabolism and behavior, seems to be required to assure optimal outcome as well as identify gaps in care continuums, although the essential role of preparing and managing the home setting to mitigate risk factors seems to be a function that every care subject requires regardless of age, health status or level of impairment.
Hello.
It would be difficult for any practicing provider to provide the information here, in a professional capacity or otherwise. It is not presented here if this researcher is a practicing provider. The answer make not make anyone reading this particularly comfortable. However, I was educated at a university with a large teach hospital, specialty care and primary care graduate medical education institution. Researcher learned this pathways on an information technology teams with a diverse group of health industry worker where credentialed in diverse nuances of clinical, primary, specialty, mechanical and molecular levels of therapy and care. 2 1/4 decades of tracking molecular pathways in this regard. Researcher has graduate, undergraduate and certificate education credential in arts, science, technology, and in industry level data, analytics and administration.
Also, the researcher has participate in care processes. One such instance included performing as care liaison to manage interaction between a care subject and practicing clinician for disease involving atypical proliferation of cellular entities. Forgive the euphemism. The practicing physician was open, communicated freely what their analysis was and what therapies were being used for what reasons. Interactively, the practicing physician and researcher were able to ascertain that every version of disease of atypical cellular proliferation, typically known by another commonly used name that most are familiar with, required both the inhibition of PEMT and upregulation of Choline Kinase. Thus, the adjuvant therapies being selected, inhibitors of Aromatase and inhibitors of Estrogen Receptors, each would enhance the cause of the disease. The aromatase therapy was decreased to 1/4 of what was already being prescribed.
Subsequently, the research and the practicing physician were able to ascertain that the calficiation deposits observed in the condition were the result of pH levels being impaired in the microenvironment, used of antacids that were providing Calcium Carbonate, resultant of Oxalate deposits resultant of Hyperoxularia linked to diabetic pathology, and each were exacerbated by electrical signals being presented by Cardiac Pacemaker implanted in the tissue where the condition originated.
Additional analyses revealed that not only was Cardiac Pacemakers producing electrical fields, but the environment was inundated with wireless communications, uncovered electrical outlets, mobile communications devices, and appliances. The industrial, clinical and health and safety information clearly presented inducible nitric oxide synthase as an inhibitor of PEMT caused by these diverse fields along with energy being emitted by the pacemaker. Also the ponderomotive effect was found to cause asymmetric flow in vascular areas that results in deposits along the vascular wall, resultant of electrical and magnetic fields. Thus, iNOS was depleting intracellular calcium, poking holes to deplete endoplasmic reticulum and extracellular Ca2+/L – Arginine, as well as causing collapses of the sarcolemma, amoeba shape of cellular entities, impaired metalloproteinase activity, deterioration of the extracellular matrix, depletion of myelin basic protein that requires L-arginine, sequestering away L-arginine and Ca2+ away from eNOS and nNOS, as well as causing systemic gradients in Ca2+ being depleted from bones because of such strong iNOS signaling. These factors also potentiate intermittent infarct activity as uncoupling of any of the NOS enzymes, including vascular pathology from eNOS impairment, vascular pathology from deposits along the soft tissues and among vascular pathways, calcification from detrimentally enhanced calcium in circulation, intermittent dementia from uncoupling of eNOS/nNOS, and exacerbation of diabetic pathology as energy fields enhanced renal iNOS and impaired renal eNOS/nNOS.
Energy protection dots were placed on the windows of the home near electricity and communications wiring, in the direction were electricity tranformers and electricity substations were located. Also, electricity plugins or power outlets were covered with duct tape and a energy depletion capability for the bed was devised that also included a grounding wire suspended over the bed, both of which were then linked by a wire to a long metal artifact that was extended into the ground.
Care activities were then expanded to the primary care physician whom was equally open and capable, although there was already being implemented ways of managing PEMT pathways at this level.
After reconstituting the PEMT pathway including Choline, Phosphatidylcholine, Trimethylglycine, Folate, S – Methylmethionine, Glutathione, cystathione, Vitamin Supplement and mineral supplement, the multiple times per month visit to the Emergency Departments no longer occurred, the patient improved from immoble to being able standup up and walk with support, see over long distances and exhibit spontaneous recall along with spontaneous expression of specific tastes, asking for specific foods, and conversion that included required analysis, thinking, and memorizing cognitive concepts for extended duration. B12, B6 were also specifically included. Superoxide Dismutase, L-arginine, Catalase, and N Acetyl L Cysteine, all were included. Berberine and Curcumin were also included.
Kidney stuff was then utilized to help stabilize Hyperoxaluria, Bottled water was already being utilized to avoid Chlorine/fluorine and particulate, which are also sources of iNOS.
The specialty care health provider then, after several follow up instances, completely removed the inhibitor of estrogen, with the requirement that complete supplemental regiment be continued, sources of Carbonate in therapies, antacids and foods were to be kept to a minimum and vitamin K2 be utilized to prevent calcification of soft tissue by managing the increased Ca2+ levels resultant of iNOS activity.
Over the long term for the nonagenarian, more than 90 years old, the only time an opportunistic microbial condition occurred and every instance in which a visit for emergency care occurred was after a week or more lapse in implementing the regimen along with exposure to energy fields outside of the protective fortress built to manage detrimental influences.
This model, clearly presents that a role is required for each patient in which assuring of these foundational pathways occurs interactively with specialty care and primary care. During the complete duration of improvement, the care subject did not every fully receive the recommended dosages for the supplements because of social, cultural and logistical issues which cannot be elaborated upon in this context.
These suggest that modern medicine seems to be inadequate only because it requires that the foundational nuances of metabolism, biology and physiology be mapped, assured and analyzed to find gaps in therapy as well as inadequacies in physiology.
Choline was already being supplemented in small amounts requiring less reliance upon insulin injections and more stable conditions, but the choline supplement include Calcium carbonate and other factors that were actually included in the deposits linked to exhibition of atypically cellular proliferation. Choline supplementation and Kidney Stuff stabilized the disease and regressed the level of Kidney pathology.
Although the status quo for the care subject could be indefinitely sustained in this context, assurance of the recommended dosages would caused regression to independent function for the care subject.
The omitting of visits to the Emergence Department, however, revealed gaps in care continuum because physical therapy, nutritional support, skilled in home care, occupational therapy and physical therapy, all were only linked to episodic visits to the emergency department. Thus, it was clear that care systems like other systems were having a difficult time integrating these capabilities and this N – Tiered full stack application of their resources unless being galvanized by an Emergency Room visit and admittance for inpatient care.
The opportunities for care continuums to be independent of if care and continuums emerge from or are conducted in inpatient, outpatient, office visit or home setting is imperative in this instance. While, also, an independent, objective, clinical role that manages care in all of these settings by setting and assuring a foundational basis for biology, physiology, metabolism and behavior, seems to be required to assure optimal outcome as well as identify gaps in care continuums, although the essential role of preparing and managing the home setting to mitigate risk factors seems to be a function that every care subject requires regardless of age, health status or level of impairment.
The care subject had a multigenerational support system that had evolved over nearly 4 decade of diabetic care. Regular instrumentation of diagnostics and care, along with logs of diagnostics were being implemented. The community had come to also support each other in numerous ways include assisting transportation, care, providing essential factors used to sustain quality of life. Not many groups have been able to sustain such level of care. Thus, regenerative priorities and processes that regenerate cognition, physiology, metabolism, occupational function and physical function, have to be integrated to relieve resource requirements for clinical works and groups providing care for health subjects. This means that civilizations should be coming full circle in their priorities, investing in health, wellness and a focus of its systems on enabling, sustaining, regenerating and assuring vital being and optimal physiological/cognitive function.
Another important area of therapy for this care subject emerged as management of trimethylamine-n-oxide, which emerged in the literature and data as the number 1 cause of sudden adverse health events, including abated vital being wrongly described as occurring resultant of natural causes. The clinical data and histology data was use to ascertain the role of PEMT inhibition in all manner of disease involving atypical proliferation of cellular entities, while also revealing that trimethylamine-n-oxide was involved as a causal factor in sudden adverse behavior, dementia, behavioral health conditions, and was the number one cause of stroke. Therapeutics used for stroke, including super clotbusters or thrombolytics such as TPA(produced naturally by PEMT anyway when it produces PMME, PDME and PC) go after an ancillary factor in sudden adverse vascular events and vascular pathology.
Trimethylamine-n-oxide exacerbates choline deficiency by impairing transit of choline from digestive pathways into physiology while causing activation of platelets and foam cellular entities, although the primary pathology was presented as causing vasoconstriction in numerous areas of anatomy constituting the pathology pattern in many diseases and for vascular adverse health events. However, trimethylamine-n-oxide also could be produced as the culmination of uncoupling of Nitric Oxide Synthases where impaired NOS produces superoxide, which becomes H202 from Superoxide Dismutase activity, followed by production of H20 by catalase but catalase is impaired first reversibly and then irreversibly by Homocysteine, S-Adenosyl Homocysteine and Homocysteine derivatives such as Homcysteic Acid and Homocysteine, Thiolactone. Peroxynitrite emerges as some of the NOS activity produces Nitric Oxide, resulting also production Hypochlorite along with producing trimethylamine-n-oxide. This uncoupling pattern is also accompanied by inhibition of PEMT, upregulation of Choline Kinase to produce Phosphocholine that can activate platelets.
These factors can suddenly or progressively impaired vascular plasticity including being diagnostically indicated by Ultrasonograph measurement of Carotid Intima Media Plasticity. The literature clearly linked Carotid Intima Media thickness and plasticity to risk for sudden adverse vascular events, ischemic and hemorrhagic, as well as dementia, impaired vision impaired motor function and all manner of neurological pathology.
The best way to measure trimethylamine-n-oxide was indicated as specific gravity of urine, or Ultrasonagraph of Carotid Intima Media since the only known way of repairing Carotid Intima Media Plasticity or thickness when in pathophysiological ranges was presented in the media as managing trimethylamine-n-oxide. FMO flavin monoxygenases are known to be modality producing trimethylamine-n-oxide from digestive pathway trimethylamine.
A continuum of therapy was devised interactively with the primary care provider. Trimethylamine-n-oxide is produced from trimethylamine or from uncoupling of NOS. Trimethylamine sources emerge from eating meat, chicken, eggs and fish or choline dense foods particularly phospholipids such as phosphatidylcholine, such that small amounts these become impeded during digestions and less than optimal digestive pathway microflora reduces these to Trimethylamine.
A broad spectrum antibiotic during any sudden adverse health event or a phenotyped antibiotic during an emergency specifically competent to any microflora proliferation, is recommended. Also useful are these. 33DMB which counteracts the serum or circulating nuances of the pathology, including managing foam cellular entities, platelet activation and other factors. Management of C – Reactive Protein because it inhibits PEMT similarly the inhibition of PEMT by trimethylamine-n-oxide. A regular laxative. A Probiotic. A prebiotic. A Post Biotic. Living foods such as yogurts or living foods such as fresh salads or raw living foods. Grapeseed oil or Grapeseed Extract. Olive Oil, fruity extra virgin versions. Balsamic Vinegar.
Every entrance into the emergency department was required to be accompanied by these factors are frontline therapies. These were instrumental in preventing sudden adverse health events and progression of pathology. Also, however, when progressive cardiac myopathy was diagnosed in multiple instances and it was prognosed that the care subject would not be able to leave the urgent care setting ever again, a conflict emerged in each such instance in which the probiotic Align, along with Olive Oil and Choline and Kidney stuff, as well as a few of the other factors were allowed to be instrumented in the care setting. In each such instance, the care subject was released after all diagnostic parameters stabilized.
Thus a list of 12 to 20 factors was derived as reasonable inhibitors of PEMT and the list was taped in plain view of clinicians and health professionals in the admittance room where the care subject was placed. Each clinician was asked to diagnostically assay each of these and manage them or let supplements be brought in to manage these. In each instance, only after it was considered that there was nothing else that could be done, implementation of one or more of the therapeutics devised with the specialty and primary care providers result in release of the care subject to the home setting.
Finally, the care facility devised a coumadin clinic that instrumented Turmeric or Coumarin, resulting in stability because Tumeric manages about 5 or more of the inhibitors of PEMT.
However, clinically it emerged in care as was confirmed by the literature, that methionine, folate, or turmeric, each were not able to replace a required obtainment of 1326 mg of choline each day. Below this level, aging factors progressed, deterioration of inherent, adaptive, humoral and cellular immunity centers emerged, opportunistic microbial disease emerged, and only choline improved these.
The national health systems produced an advisement to all health facilities presenting that inpatients must be provided choline supplementation because if such supplementation was omitted, choline deficiency or choline inadequacy enabled opportunistic microbial diseases, including development of nosocomial microbial disease of resistant nature, including hepatic deterioration, thymic involution, and other pathologies would likely emerge as the primary cause of complications or abated vital being. Correlative to incurring this advisement, the American Medical Association released a recommendation for Choline Supplementation to support Maternal health, gestational health and breast feeding. These events occurred two decades of after Choline was added to the list of required nutrients, in tight synchronization for discontinuation of funding public health facility construction by the Hill – Burton Act, circumventing the requirement for publicly funded hospital facility construction or resource additions to be verified with a demonstration of bona fide demand in the service area of such prospective construction.
The discontinued funding of Hill – Burton circumvented requirements for certificates of need for health facilities, disabling a governing mechanism to Roemer’s ‘axiom’. Roemer’s Axiom is the dynamic in which adding additional health facility resources in an area results increase occurrence of disease, adverse health events, mishaps, and abated vital being. thus, once choline was added to the list of nutrients, the cause of the increase in abated vital being resultant of hospital construction had already made it to the list of required nutrients or was in process of being added. That causal factor was choline deficiency and factors that inhibit PEMT, thereby impairing a primary pathway for de novo choline synthesis within anatomy.
However, these events did not limit private construction and development of health industry business otherwise, as well as moving production of health services capabilities and resources outside of service areas and to other civilizations. The result was increased influence on systems of this civilization because organizations and systems producing health resources have to make revenue and move their products along supply pathways in order for revenue to be obtained, workers to be provided financial resources and workers as well as those whom workers are affiliated with to obtain the resources required to meet human, social, behavioral and physiological requirements.
Abatement of Healthcare Certificates of Needs requirements came in reasonable synchronization with the first corona microbial pathology events the late 1990s and early
Also, it is known that the moratorium preventing the utilization of abated vital being as a sanction resulted in at least a 20,000 decrease in occurrence of abated vital being that would have likely reached 100,000 or more decrease each year, if the moratorium were not concluded right as the decrease was steepening. Mishaps, detrimental events involving system workers, all were decreased also, while average span of being reach new all time levels during the moratorium.
The abated utilization of certificates of need coincided with emergence of corona pathology while such disease would be of specific relevance to the kinds of disease that would increased resultant of mitigated influence from the Hill – Burton Act Provisions. Moreover, at the National level, a moratorium was implemented on the use of abated vital being as a sanction, resulting in a gradual decrease of the number of instances, detrimental level and risk from corona microbial pathology.
However, within one month of this moratorium being concluded or deactivated in 2020, the corona microbial pathology emerged as a pandemic, and it affected the global populations similar to how the moratorium preventing utilization of abated vital being as a sanction resulted in decreased levels of abated vital being not only in this one instance of civilization but resulted in similar decreases instances of abated vital being in almost all other civilizations of the world.
Implementing abated vital being as a sanction, allowing distribution of artifacts specifically used to abate vital being, and not prioritizing, managing and therapeutically intervening the factors that cause inhibition of PEMT, all inform the universes of a deprioritization of Humanity which conflicts with the inherent priority that universes have afforded Humanity as the culmination of its creative forces.
Interestingly, Betaine homocysteine methyltransferase 2 which metabolizes S-Methylmethionine and homocysteine into methionine and dimethylglycine utilizes S-Methylmethionine as a substrate. S-Methylmethionine has not, at this instance, been found to be de novo synthesized in human anatomy. This contexts mimics rubisco in that these both, if excluding the obscure reference to Human Rubisco enzyme and photosynthesis occurring in Human anatomy resultant of Neuromelanin in the substantia nigra as well as melanin otherwise, bring external metabolism from the environment into physiology, confirming an integration of physiology with the environment. Perhaps only digestive pathway microflora and synthesis of trimethylamine as well as PEMT synthesis of PMME, PDME and Phosphatidylcholine to scrub the environment with powerful antihistamines, otherwise present compelling examples integration of physiology with the environment. Statistically, however, there may be numerous population level correlates in systems of civilization that present integration of physiology and anatomy with systems, such as Roemer’s axiom.
BHMT2 activity using its substrate, S-Methylmethionine, protects hepatic tissues from injury during challenge from toxic levels of Acetaminophen. Hepatic challenge with excess Acetaminophen can be managed with N – Acetyl L Cysteine, such that the mechanism of impairment seems to be depletion of hepatic Glutathione. The depletion of Glutathione is described by the 10 times lower availability of one of the substrates for GSH synthesis known as L – Cysteine when compare to other precursors L – Glutamate and L-glycine, describing also why its CoFactor Magnesium along with Glycine as Magnesium glycinate are utilized in therapy for oncology of the breast. This suggests also why Se-Methylselenocysteine is useful in therapy for oncology of the breast.
BHMT2 utilizes SMM or S-Methylmethionine and homocysteine as its substrate, producing H+ and Methionine. Plantae exhibits endogenous synthesis of SMM from Methionine, while SMM de novo synthesis is not endogenous to Human physiology, according to the literature. However, even though SMM is indicated to be obtained from Plantae to activate its Humans enzyme for catalytic activity, the literature observes that BHMT2 plays a protective role during noise challenges and even compensates or rescues BHMT inadequacy which results in substantial impairment to hearing after noise challenges correlative to age. The conclusions here are specifically important because suggest clearly that the Human status quo at birth was not intended to wholly determine its circumstance or duration of being, clearly having physiological mechanisms intended to achieve somewhat indefinite sustainability. Similarly, these clearly present that an important role for humanity includes its physiological oneness with biome, complimenting its physiological oneness with universes through the systemic integration of Hydride required for conscious cognitive ability.
It is somewhat confirming, the BHMT2 enters an H+ when depletes Homocysteine, adding H+ that is opposite to the managed levels of H- when comes to energy balances, while its synthesis of Homocysteine enters an important manner of managing carbonate in the carbonate buffering systems comprised both of Methionine and Cysteine in Methionine. Most importantly, these more strongly elute reason, meaning and balance within physiology, among systems of the universe, between the biome and the Universe as well as amid the cycle of Hydrogen that begins with light or energy causes H2 to become Hydrogen fractals that search for one another among the Universes causing the synthesis of all the elements of the periodical table. Fractals are rejoined in a managed and directed way by systems of physiology to produce ATP. Perhaps it is ATP that most indicatives Life among the universe because it enables entities or loci of biology to perform activities in directions opposite to the gradients that exist in the microenvironment and macroenvironment, giving way to individual interest and self-interests, as well as individual priorities among organisms, species and aspects of biology within species.
Reference. FACEBJ. Volume 33. Pages 5942 to 5956. 2019.
Reference Genome Res. Volume 20. Number 1. Pages 28 to 35. January, 2010.
The relevant events of this era, seem to be occurring for reason. The ages are asking and even requiring populations and leadership to make common sense conclusions about incomes, reducing these to empirical causalities and mitigating, preventing or managing these causalities, regardless of the subterfuge, obfuscation, and inability to trust that such changes really are in the interests of all humans. Each time such an affirmation of Life occurs, instead of being mired in obfuscation, such empirical causalities reveal something pivotal, transformational and moving.
What does it imply when optimal health, cognition and behavior is integral to oneness with the Universes, timeless oneness with the Universes, while when such oneness is impaired through dissociative processes or influences, then the biome rescues this oneness by reconstituting it through enhanced PEMT integration of Hydride into physiology?
If policy, procedure, construct, or artifact cannot be distributed among populations, implemented or applied without potential of abated vital being, then why are these being allowed to be synthesized, distributed, implemented or applied? If a concept suggests that Humans were intended to incur vital being, then why are there so many suppressed, unutilized and potentially transformational capabilities potentiating outcomes otherwise?
The inclination to limit Humanity and impair vital being, as well as allow the Human experience to be diminished without reason, certainly are not being derived from, imparted by or suggested by the favor of the Universes that has allowed Humanity to emerge, persist and progress.
Systems were intended to enhance the achievement and realization of the favor of the universes, because being Human, means that these are already inherently yours.
The same care subject obtained a topical reaction to a antibiotic, used to assist in microbial challenges emerged when choline supplementation was either omitted, refused during instances of strong cognitive awareness, as well as resultant of the incomplete level of choline which should have been, 1,327 mg per day, but was less than that, even when included nutritional obtainment. Choline levels have to be stabilized over time because only about 5 percent of choline from food makes into into circulation and even this is impaired in the microflora incompetent digestive pathway.
However, the rash was treated with by comprising the choline oxidation pathway supplementally, and using the same factors for a topical capability integrating into typical skin lotion. However, the BHMT2 substrate S-Methylmethionine sulfonium or SMM was added at 400 MG per 8 ounces of lotion, while other factors were added to to a bottle of lotion having about 24 ounces of fluid.
The topical solution was intended to ameliorate itching, such that aveeno skin lotion was mixed in at about 6 ounces per 24 ounces of lotion.
The mixture was able to allviate topical itching. However, the skin reaciton had raised patches of irritation, that were reviewed by home care nurse and primary care physician and confirmed to not require advanced care.
The raised patches were amid scars and other tpical markings that were recent and some were exhibited for nearly 70 or 80 years. The raised patches were covered in about 4 by 4 squares of gauze treated with the lotion. The patches were left in place for about 24 hours at a time. Then for about 48 hours at a time. As the raised patches started to abate, the guaze was left in place to dry in place. Removal of the last few square gauze patches revealed something remarkable. The patches of reaction had dried and peeled away from skin, as did many of the scars that had been in place for nearly 8 decades. Some of the peeling away was incomplete, so the patches were reprovisioned and put in places for several more days. After which, air drying was allowed. some of the scars and reaction areas fell off by themselves. Others could be remove carefully by peeling these way. Some such areas, however were include, so peeling was able to remove some but not all of the scar tissues.
No interest was expressed in completely removing all of the scars on the exterior of anatomy, even though this was suggested.
S-Methylmethionine is substrate for BHMT2 which is a Human enzyme but its substrate is not known to occur in physiology except in ingesting high sulfur vegetables and foods, particularly plants which produce SMM from Methionine. This suggest a time when mammalian physiology experience increased levels of sulfur in the environment and exhibition of SMM in the environment. This physiologically link Human original nutrition to Plantae and absence of Plantae in nutrition disrupts a major biosynthetic, regenerative and repair pathway.
However, importantly, because Vitamin U or SMM was accompanied by remarkable stability in all manner of physiological diagnostic indicators in this therapeutic context, and was assisted by comprising the nuances of choline oxidation, while the complete PEMT pathway was not ever comprised in this therapeutic context, leaving even more remarkable repair, regenerative outcomes and stability as potentialities and to the imagination, one conclusion was able to be verified. The same manner of repair of scar tissue must have been occurring within physiology and among tissues, these were causing somewhat confusing paradoxes to occur.
One of these were low blood pressure and low pulse rates similar to advanced athletes at rest without any manner of symptoms, which, unfortunately, occurred in a context of pacemaker activity. These suggested that mechanical interventions such as amputation, resection of tissues or anatomy, as well as prostheses, could force an election to occur about regenerative care. At least once instances exhibited admittance of the care subject for asymptotic low heart rate and low blood pressure, with inconclusive results, not dementia, no impaired cognitive activity, and continued stable low blood pressures, which only increased once inpatient care had prevented the instrumentation of the therapeutic regimen long enough for some of the pathologies to become reconstituted. However, the coumadin stability clinical interventions prevented these from progressing to accumulated hematopoietic fluid and coagulation anomalies, while certainly it would require weeks to regress the benefits of the therapeutic regimen.
The most substantial risks in the care context were these. Holidays or omitted instrumentation of the regimen. Inpatient care which does not allow outside therapies to be instrumented, such that patients are caused to incur the statistical outcomes that are competent to their typical care pathways. Consistent coverage of home care, occupational therapy, and physical therapy.
Everything that is occurring, even when less optimal, merely present information about Human inadequacy continues. Thus, because any system naturally elutes information about inadequate achievement of its objectives, so does any system founded or coming to prioritize Life, Liberty and Pursuit of Happiness.
There is hardly anything more Human than to produce systems that require of humanity more than is required of them nature. However, there is also hardly anything more human to ask of oneself that which satisfies or confirms such bias toward excellence and the exceptional.
Thus, are the progressive nuances of civilization that emerge as dissent from the status quo and cast, farther, the nuances of Liberty through their founding priorities, each but the product of the nuances of civilization from which they emerge? Are the successes of such civilizations theirs alone, or are these integrally shared by all civilizations and all in the span of the Human experience? The Patriot Kossuth questioned if Liberty, indeed, belonged only to one civilization, or if it was the integral inherent affordance for all among Humanity. J.F.K. would utilize Kossuth in describing why reaching the moon was so important, describing not only that is hard from difficulty perspective, but that is was hard from P Hardness standpoint in affirming Humanity’s existence among the Universes. Thus, are the leaders of Civilizations founded upon the Context of Life, Liberty and Pursuit of Happiness, likewise, that Civilization’s Leader alone?
Thus every outcome has to be considered in the context of if it could have, would have or likely may have been exhibited in nature without the enculturated nuances of biases, distress, inadequacy, and 12, 20 or 50 or more factors which shape or inform Human outcomes in civilization. The disparities, therein, are information and are the ways in which the ages speak to advocate for ever increasing satisfaction Human requirements, social requirement, and confirmation of Human existence among the Universes.
Are systems the problem, or, is it that systems of the universe and the ages themselves are providing information that is not being translated efficiently into change that benefits Humanity? Civilization’s in which massive nuances of the population are endeavoring upon paths of excellence, changing what occurs in the future as well as changing what has already occurred by achieving such excellence in nonpolynomial deterministic contexts, inherently potentiate the diverse outcomes observed in civilization including those outcomes which are less than optimal.
Thus, in closing here, it can be asked if civilizations founded upon the contexts of Life, Liberty and Pursuit of Happiness do more than merely prioritize the assurance of thereof. Do such civilizations elute a space or context in which the degrees of freedom are enhanced, increased, or relaxed in way that was intended for humanity to confirm that the culmination of its creative forces, the favor that is requisite to such creative forces, and the exhibition of Life, Human Life, indeed, was worth its infinitesimally improbable occurrence? Is the Cinderella story in any context, particularly the most improbably Cinderella story of the Universe, the exhibition of Homo Sapiens more about what is done with the opportunity to promote to Universes level prominence than it is about any such achievement?
Indeed, civilizations founded upon the priorities of Life, Liberty and Pursuit of Happiness, connect Humans more directly with the empirical nuances of reason, connect Humans more directly with the impetus for civilizations, confirm the impetus of Human existence upon a Universes Level stage. It is upon such Universes Level stage which great acts and achievement that confirm Humanities existence are potentiated. Thus, among Generations of Humans exhibited in this context, as well as Generation of Humans affected by such context, all is changed in such achievement in a way that was meant to be information enabling the greatest of achievement which is the confirmation of Life itself, the appreciating of Life as the creative forces of the Universes, and continued, endless, beneficent and productive reach for the stars.
Republics and Democracies are not impugned in any of these observations and analyses, for, indeed, democracies are as a people implement them.
Merely because a group of Humans come together and present their agreement to produce and implement a social construct, using some system by which the construct is either affirmed or not confirmed, does not at all constitute a Democracy.
Similarly, merely because people presume, assume and practice power over the affairs of a civilization, does not constitute a Republic. Clearly, even in what was the most humanistic of foundations for an emerging civilization, that is Life, Liberty and Pursuit of Happiness, did not inherently prevent the implementation of abated being as a sanction resulting in 20,000 to 100,000 instances of unnecessary collateral instances of abated being each year. Observing that such a Republic or Democracy might cause massive levels of oppression, abated being, and tumult, including cause a population to abrogate itself by implemented abated being as sanction in way that results in 20,000 to 100,000 instances of abated vital being each year, as instances of the Human experience have presented, makes it reasonable to understand that a Republic and a Democracy require more than mere Majoritarian social dynamics in a Republic in which the power for decisions are derived from these same population exercising Majoritarian systems of making decisions.
Thus, a Republic and a Democracy, in order to be a Republic and a Democracy, must link its priorities, decisions, outcomes to incipient nuances of reason. The power provided to the populace cannot include the power to abrogate the populace itself or humanity itself. A republic cannot dissociated less than majoritarian nuances of the population from the favor of the Universes comprised of assurance of Life, Liberty and Pursuit of Happiness merely because most of such a population disregard the Human and Civil rights of another group. A Republic and a Democracy cannot be comprised of decisions made by the uniformed, less than aware or otherwise unknowing perspectives, or inaccurate opinion, which, when implemented through Majoritarian Democratic Dynamics, results in massive unnecessary detrimental behavior, detrimental physiological outcomes, abated vital being, and undue complexity and scapegoating of particular nuances of the population. Imposing such outcomes among others and among themselves, clearly demonstrates that a Majority opinion can result in massive detriment to a population.
The definition of a Republic and Democracy has been too loosely utilized in the span of the Human experience. Thus, the way in which merely implementing a Republic and implementing a Democracy, has been expected to result in resolution inadequate and less than optimal social, economic, behavioral, social and physiological and Human outcomes, has been a disservice to Republics and Democracies. Humans and systems must foundationally and continually link the decisions in Republics and occurring within Democratic systems to incipient nuances of reason. Life, Liberty and Pursuit of Happiness seem most empirical in observing that civilizations were constructed to elute Human sustenance in a focused, control, directed and sustainable way, from nature. Systems were not intended to be utilized to impose complexity and difficulties upon citizens and workers, particularly when these are unnecessary. Systems were intended to implement the Golden Apple of objectives, Life, Liberty and Pursuit of Happiness, while themselves exhibiting activity the mimics biology itself, becoming ancillary nuances of species DNA that asserts Human priority among the Biome and among the Universes. Every social construct and decision in a Republic, as well as every political outcome, requires analysis to observe that its effect is beneficial to Humans, assures Life, Liberty and Pursuit of Happiness, and only might limit these in a comparative Liberty interest that expands Liberty where it might otherwise be assured.
Reason, also requires that every outcome be considered in the context of its empirical causalities instead of being attributed to those incurring outcomes, conveniently excluding disjoint, Boltzmann dynamics in which the most empirical and causal factors are at quantum, atom, molecular and temporally distant loci. Republics, thus, require observation, analysis, and understanding of Human outcomes and effect of systems themselves, in a way that does not every exclude the imposition of nuances of reason in any outcome. A species abrogating itself, through group dynamics or inclusively, cannot ever be consistent with reason, a Republic and a Democracy. Republics and Democracies are defined by their service to Humanity and the level to which optimal Human outcomes are assured. The characteristics of the implementation of a Democracy, thus, seem flexible and secondary to the ability of any such arrangement to assure Life, Liberty and Pursuit of Happiness.
It is not difficult to observe that the Wisdom of the 1770s and, indeed, the wisdom of the emerging Human Species in its first exhibition upon the earth, wherein Life was the priority of all activity and emerging social capabilities, seems to have become dissociated from absolute priority in systems of civilization. Every detrimental outcome that now, in modernity, emerges, can be linked to the inadequate exhibition of Life as an absolute priority in all systems of civilization. Of course, these include the utilization of systems to manage or mitigate circumstance when Life is affected by a competing Liberty interest, in a way that benefits all those who might be involved in such circumstance beneficially.
Clearly, the 12, or 20 or more factors that inhibit PEMT were intended as mechanisms of sensing the environment, including factors that are consciously unascertainable, such that a change to perception, cognition, function, and behavior occurs to cause disruption of behavior that enables migration, obtainment of shelter, disruption that causes change, or some other way of enabling populations and species to survive when detrimental circumstances occur. These susceptibilities are intended to cause change, analysis, learning, introspection, obtainment of knowledge and wisdom to make changes to the status quo to sustain humanity. Systems of civilization are pervasively managing detrimental outcomes which are being caused resultant detrimental influences, the 12, 20 or more factors, the 50 or more factors that shape these into the outcomes observed in civilization, and which occur because systems of civilization so strongly mimic in function and jargon the foundational nuances of genetics and lipid chemistry within which PEMT pathways are situated.
Systems of civilization, like any systemic algorithm, routine or systemic group of processes, natural have an effect upon the contexts in which these are performed, resultantly producing outcomes that are shaped by such dynamics, elute the causal mechanisms for which detrimental outcomes occur, elute as information and Human outcomes disparities in achieving objectives of such algorithms, and produce as information and human outcomes correlates, associations and other factors that enable systems to improve the human condition.
Every system in the universe, correlative to its duration of exhibition, has a propensity to prioritize itself over its incipient circumstance, incipient status, other systems and over humanity. This may be a foundational unified theory applicable to quantum, atom, molecular, metabolic, anatomical, physiological, perceptive, cognitive and behavior, as as well as environmental, biome, planetary, solar system, galaxy and universes level systems. It does not seem to be important if such propensity for self prioritization produces sustainability or increased duration of exhibition for a system or if it is the comparative increased duration of exhibition that results in such prioritization of a system over other systems, particularly those which have become abated or no longer exit. What is clear is that systems have a paradoxical propensity to elute information while pervasive nuances which are eluting such information may seem to be in a quagmire. A very Senior role in a region which does not use abated vital in a civilization founded upon the constructs Life, Liberty and Pursuit of Happiness, for instance, was able to manage that region’s resources to abate massive levels of detrimental outcomes that was cursorily attributed to decreasing synthetic electromagnetic by nearly 15 percent or more. However, the Senior member of the regions leadership was involved in a scandal involving reproductive contexts, eluting information that would cause the population to produce increased levels of Hormones resulting in enhanced expression of PEMT. Such a Senior Role and the performer in such role also was linked to suppression of information about increased levels of detrimental outcomes occurring care centers for the aged. Such suppression invariably would have resulted in decrease in homocysteine, enhancing PEMT availability, because distress, apprehension and effect of release of such information is known to increase levels of homocysteine among populations.
Thus, the reason that it seems that progress is not being made in assuring Human Life, Liberty and Pursuit of Happiness, is that the systems which are being observed in this capacity are distant from the nuances of systems which must acknowledge the 12, 20 and 50 or more factors, changed all social constructs to focus these as causalities for detrimental outcomes, locus of change to prevent, alleviate and manage detrimental outcomes, and as priorities in all systems which manage less than optimal human outcomes, circumstance, physiology and behavior. It is certain that a screw being turned by a screwdriver or drill wonders why it is that such a drill is intend on disrupting its status or changing the status quo. Each, the screw, the screwdriver or drill, are pervasively aware only of their status and circumstance, while being unaware the blueprint and plans for the room, structure, edifice, and area from an infrastructure development perspective. The screw and the screwdriver as well s the drill, all are being asked to reconcile difference between the status quo and the objective, which is unable to be reconciled at their level because such substantial change to social constructs, systemic processes and programs may be required to prioritize the 12, 20 or 50 factors.
Systems, eluting information, can do so as information, as human outcomes and as detrimental human outcomes. Sometimes information emerges as a detrimental human outcome that is promoted into the populations’ psyche in a way that causes decrease in abated vital being during a difficult context, such as a pandemic. This propensity is why Human priority of such importance, because the performance as universes level sensory mechanisms makes humanity susceptible to all nuances of outcomes which they or others pervasively may not be able to decipher in a timely manner. Until this amazing susceptibility and how these have changed the Universes is acknowledged, systems are changed to understand human outcomes and their empirical causalities, and until humans are individually and together educated and made aware of these before , during and after less than optimal outcomes, it can seem like progress in assuring Life, Liberty and Pursuit of Happiness has bee inadequate. Indeed, however, as the information presents, great, productive, and beneficent leaps in understanding has occurred in such regard, even being integrally exhibited in the activities and outcomes of the leadership of civilizations. It is time to begin turning this knowledge into change and bending or turning the information being produced as less than optimal outcomes into the achievement of the hopes of Humanity.
The primary role of systems of civilization, particularly civilizations founded or progressing to prioritize Life, Liberty and Pursuit of Happiness, has been and is in their intricate similarity to PEMT pathways and how these mimic foundational nuances of Life itself. This role includes the prioritization of Life, Liberty and Pursuit of Happiness, as well as the Silver Frame for implementing this Golden Apple of Priorities. Such systems were intended not only to enable assuring of Life, Liberty and Pursuit of Happiness but to elute impedance thereto and document instances that demonstrate that such objectives are not being assured, resulting in impetus of observation, analysis, introspection, innovation, and change. Such change was intended to ever increasingly expand the assurance of Life, Liberty and Pursuit of Happiness.
Everything presented here is intended to increase the appreciation for systems themselves as they were intended and not how they may have come be utilized in particular nuances that seem anathema to such incipient priorities. A system allowed to impose vital being producing an cascading effect that seems to cause abated vital being to occur in diverse other nuances of its function and among populations, including becoming an impedance to innovation, progressive psyche and essential humanist cognitive processes. Senior leaders who have emerged to abated the usage of such sanctions have been preventing many tens of thousands of instances of abated vital being while the response in some instances have included being subjected to uncertainty by inability of the linkages presented here to be acknowledged and presented for global understanding.
Sometimes, because Humans are favored so highly and completely by the favor of the Universes, that in order to assure such favor, particularly when such favorable influence is being impeded by systemic nuances or circumstance otherwise, detrimental outcomes might be produced. It dos not have to be this way. However, certainly, because such a disparity seems to exist between the status quo and what is presented here in numerous analysis, sometimes humans can find themselves thanking goodness for such outcomes regardless of if these are detrimental or beneficial. The groups of people, professionals and physicians, whom were able to link events of the previous several years to decades and centuries, with precision to PEMT and Homocysteine, certainly have a reason to be thankful to what Humans in other eras have had to do make Humans in this era aware of these nuances of physiology.
You are a Human. Thus, your instance of vital being is acted out a great stage to which all of the Universes pay attention. Everything you do with this opportunity is information about the Universes, and you need only conduct your vital being each day to entertain and sustain the nuance of the universe with which you are most uniquely entangled. Life, is what matters. The believe that Life is a gift intended to be yours and intended to be indefinite is all that is required for these tools and mechanisms to be galvanized for your exploration, understanding, application and utilization.
Majoritarian Democratic Republics, all have such a susceptibility to a majority that can be controlling of social constructs, even also being able to change social constructs to their priority, as well as exhibiting diverse inaccurate opinion, bias, nuance of psyche, often unconscious inaccurate opinion, or uninformed perspectives amplified by less than empirical analysis or understanding. These susceptibilities become hidden commandeering mechanisms through which any system exhibits the inherent propensity for any system to prioritize itself over its purpose, intent, incipient circumstance and over Humanity. Thus, systems utilize these to produce scapegoated populations which maintain the status quo because presented with context of destabilizing change at economic, power, elitist, psychological or social levels, scapegoating of populations through these mechanisms which are dissociated from reason may be easier that challenging the psyche, motives, awareness and understanding of a majority. It becomes, simply, easier to believe that people different from an individual in many ways might have detrimental character than it is easy to challenge one’s own understanding and iteratively work through the obfuscation and obscured layers of systems that have cause the status quo to emerge. It is clear that systems .as they are now, in many ways, but not every way, have become a hindrance to implementation of even the humanist perspectives of the 1780s. That hindrance occurred when constructs and nuance of precedence were imported from systems in use thousands of years before were all imported as a foundation into a Humanist civilization founded upon the priorities of Life, Liberty and Pursuit of Happiness. These constructs seem to be integrally causal to the biases being produced and imposed upon human outcomes in modernity. Largely, the importing of these systems from earlier civilizations caused the same influences which these systems produced in other eras to become directed upon civilizations of modernity, among greatly increased levels of electromagnetic energy, particulate in environment, communications influence, and homocysteine produced from artificial or synthetic influences.
The crux of such hindrance seems to be mistaking of human outcomes and human circumstance for character. These seem to be integral to why abated vital being is allowed to be imposed as a sanction, why care modalities which would pervasively cause abated vital being to be prevented have been allowed to be aloof of ubiquitous instrumentation, why detrimental artifacts are allowed to be distributed among populations with massive deleterious effect, as well as why every detrimental outcome among humans is not relegated to imposing only those dispositions which benefit all involved in such outcomes including those for whom sanctions might have been or might be a possibility.
The most unproductive and inaccurate interpretation of any of the analysis in the compendium of research with which this analysis is associated may be to suggest that systems themselves or workers in systems themselves are causal to such hindrances and or causal to detrimental effect to the foundational priorities of such an emerged civilization. It is workers within systems which pervasively are exposed to exponentially amplified levels of such risk and susceptibilities. The recent response to such susceptibilities among systems workers emerging as detrimental outcomes has been deterioration of essential immunity among system workers, when such immunity is specifically exhibited because of the increased levels of susceptibility, chronic exposure to detrimental outcomes and circumstances for which social constructs have not been adequately presented to alleviate at empirical levels. Also causal to such chronic exposure to detrimental outcomes is antiquated uninformed and inaccurate opinion that sanctions and social constructs are reasonable or acceptable solutions instead of understanding empirical causality along with prevention and alleviation in a way that prevents recidivism. These limiting perspectives and inadequate resolution may be more of a limiting factor among populations than they may be among systems workers because workers within systems were at least aware of these susceptibilities enough to originally present immunity as possibility for system workers.
The homologues are strong in the characteristics of disease pervasively, when considering less than optimal factors or circumstances in civilization. The transsulfuration pathway, for instance, which catabolizes homocysteine by directing homocysteine through several enzymic translations that become increasingly irreversible, is precisely similar to processes which managed detrimental behavior and typically include increasing volume and increasingly detrimental outcomes because causal factors are not being acknowledged, prevented and alleviated. The exhibition of abated vital being as sanction, or immitigable deprivation of Liberty otherwise, might be considered as culminating factors in such contexts, even though it is known that utilizing abated vital being as a sanction increases abated vital being among one instance of civilization up to 100,000 per year as a collateral and generational effect among generational and collateral effect otherwise, while similar effect to worldwide populations is known to occur resultant of exhibition of such sanction in this one particular instance of civilization.
Again, transsulfuration pathway is expansively useful, but it prevents recycling of homocysteine into methionine and is physiologically catabolic instead of being regenerative and biosynthetic. However, the foundational metabolites produced from such catabolism, such as sulfur atoms and sulfones, are known to be recycled through the transsulfuration pathway.
It can only be presented, regarding the use of abated vital being as a sanction, that, sometimes the path to understanding what should be done or presenting a practical understanding of how things should be changed, requires a word for a contextual example for what should not be being done.
The repression of human populations based upon gender, ethnicity, origin, etc, all present strong examples that are homologues to PEMT being repressed as a ubiquitous priority in diagnostics, analysis, care and therapies. Often, the learning, understanding, and wisdom, can occur in context of inadequacy followed by change that is visible at social and systemic levels, requiring analysis, focus and improvement. Anytime a new stimulus, factor, or individual is incurred, double stranded DNA segmentation occurs in areas of the brain, resulting in required repair. This process seems to be involved in the increased size of the brain in Homo Sapiens, suggesting also that learning, understanding and wisdom involves systemic change, as well as involves a systemic level of Hydridic Capacitance that senses changes to the brain and which can map the same stimuli pattern onto the same patterns of structural changes that have occurred in synthesis of a recorded stimuli pattern.
The repression of humanity in this context seems to be less necessary than the learning that occurs as result. Again, there merely needed to be a word for the opposite for what should be occurring before it be convincingly presented and acknowledged that which should be occurring.
Clearly, these show that a Republic is not constituted of a group of humanity coming together to make decisions and managed their circumstance. A group of people who come together and make decisions merely by a majority confirmation, does not make a Democracy. A Democracy, in order to be legitimated, requires clear, immitigable Human priority, and does not rest upon Majoritarian opinion that allows mitigation of Liberty, but continues to earnestly assure Life, Liberty and Pursuit of Happiness for all among its population. Thus, the mere utterance of Life, Liberty and Pursuit of Happiness is inadequate, while it is the achievement and continued endeavor to assure these imperatives which afford legitimacy to a Republic and to a Democracy.
A particular article observes that ethnic groups or even grouping based upon cursorily observable characteristics have been utilized in particular civilizations to produce biases and these biases can be confirmed by disparities in outcomes in many areas. Genetics have been utilized to understand these disparities in outcomes, resulting also in bias in who genetics are analyzed and considered, producing sometimes those conclusions that merely confirm a genetic causalities for outcomes. However, ancestral analysis has been utilized in recently emerged analysis because these describe not only genes, but the interaction of genes within physiology and with nature in the environments which ancestors have been exposed to. Thus, biases have been a substantial factor in why nuances of disease have both occurred differently in populations as well as have not been resolved. Genetic basis for disease that is increased in particular ethnic or other groups sharing cursorily observable characteristics, has been reason to not intervene, presenting that such outcomes in behavior or physiology are somehow supposed to occur or are not able to be prevented.
The particular article in this regard is important because it observes that ancestral analysis is better indicator of susceptibilities than genetics because genetics imply cursorily observable characteristics. Essentially, ancestral analysis allows the interactions of systems with lineages of human beings to be included in analysis. The same article observes that even ancestral analysis alone is inadequate because health disparities occur differently among populations with similar genetics resultant of disparities in social, behavioral, and environmental factors. The use of genetics in confirmation of ethnicity or cursorily observed characteristics as not only mere statistically observed outcomes but as causal mechanisms, attributes causality to something which is not specifically resultant of decisions made by a human but is resultant of factors out of the control of such human, although causality for such outcome is attributed to such human anyway. The obvious question of “how can one attribute causality to an individual for an outcome that attributor already knew was going to occur, while the individual incurring such outcome was less aware of as a potentially than the statistical information was able to suggest?” can be presented.
However, the article presented in this context of observes that it is systems which are determining human outcomes, but it is much easier to say something is inherently detrimental about particular individuals or groups than it is to say that these outcomes are the result of impaired structures and processes within civilization.
The best way to understand this article is to consider a large three or four acre group of hedgerows. Apertures have been made in hedgerows in hundreds of locations allowing movement from one open tract to another open tract between the hedge rows. Different width and height doorway frames have been placed in each of these apertures, wildly differing in those who can use which door. Some of the hedge rows have deep mud in the open tracts of land between the hedge rows. The starting sign shows the word “go” in a color similar to the color of the sound background, such that it is very difficult to see especially if having impaired ability to see contracts in color or hue. Each door has a digital sign next to it that as an arrow in different colors. People are timed to see how quickly they can navigate the maze. People are chosen from different neighborhoods. Each neighbor differs, sometimes wildly, in economic status, availability of attire used in mud, availability of shades, ancestral diversity, health status, average height, and physiological shape, as well as health status. The study might conclude that particular height people with preference for attire useful in in mud, particular height people with particular color shades and substantial economic means, or people of particular girth with other colored shades who are impaired in perceiving color contrasts, all are best cognitive and physiological groups in civilization. However, study has somewhat completely contrived these outcomes by the way it has structured the maze.
Civilizations similarly impose the same manner of thousands of complexities that impose multiple limitations, advantageous, and stimuli that are used in every decision made by Humans. These produce outcomes that are pervasively contrived and which pervasively purposefully impose those outcomes that confirm with biases exhibited in the status quo. A fast, tall, genius from an area without a shade store, would be excluded from participation in those programs and activities for which they are exceptionally advantaged, all because of the structure of study. Exceptional people, either inherently or in how they focus or apply themselves, thus, would be excluded from participation in activities or programs for which they are advantaged. These exhibit how civilizations impose health statuses and behavior upon its populations. Often, these merely confirm perspectives imported along social constructs that have been imported from hundreds or thousands of years ago into the humanist context of systems of modernity that exhibit nuances of choline and PEMT pathways in their structure.
This example does not mean that systems are not capable of producing exceptionally optimal outcomes, because systems are able do so. This does not suggest that people selected by systems are not exceptional, because such a system has selected nuances of exceptional populations. However, the imposition of detrimental outcomes is an equally important metric to monitor and understand. Such a maze represents a system that might be utilized to select exceptional individuals along side the imposition of maze without such complexities or limitations. Such a maze would be somewhat relevant if the activity for which the candidates were being selected for were sure or likely to exhibit precisely these same limitations or factors, although surely, training and equipment could be utilized to enable those performing less than adequately in any regard within this context.
Reference. Genes Don’t Cause .. Health Disparities, Society Does.” The Atlantic. April 13, 2015.
Important news. BRCA1 gene inhibits potential for impaired proliferation of cellular entities and correlated disease. The literature confirms that impaired function or genetic impairment of BRCA1 is strongly correlated with impairment also of PEMT enzyme function or silencing of the PEMT pathways. Like a march to geopolitical conflict, or emerging of disease when Glycyolysis is upregulated without also upregulation of PEMT that is known as Aerobic Glycosysis or the Warburg effect, the silencing of PEMT is like the silence of the Lambs or silencing of the Doves. This is important because it shows that the almost countless number of scenarios that can exist at metabolic levels to result in diseases involving impaired cellular proliferation, almost that is, dovetail like almost all disease and all most all proliferation disease, if not all of these, share the requisite impairment of PEMT, downregulation of PEMT, impairment within PEMT pathways, or impaired integration of hydride into phospholipids and phosphoethanolamines, correlated to increases in homocysteine, homocysteic acid, homocysteine thiolactone or s – adenosyl homocysteine.
As cohorts or groups progress in age, these provide insight into all disease, and using CRISPR Gene repair, enzyme replacement, supplements, nucleotide supplementation and other factors, pervasively, disease of all manner are becoming preventable, able to be alleviated and able to have detrimental outcomes repaired or anatomy regenerated.
Bend your goals, objectives and aspirations to become increasingly in alignment with a priority of life, ones own, those whom you are associated with and humanity inclusively. If doing so, then soon, there will be milestone in which the sustainability of human vital being will be assured. If you are in the health industry, don’t be discouraged by what you hear and what you read. This information is the residue of your efforts. If you work in systems of civilization, be likewise encouraged, these are also the results of your persistence, endurance and assuring of a space, region or context in which it is possible consider a world without detrimental outcomes and disease.
(PDF) BRCA Genes: The Role in Genome Stability, Cancer Stemness and Therapy Resistance (researchgate.net)
https://www.researchgate.net/publication/333853541_BRCA_Genes_The_Role_in_Genome_Stability_Cancer_Stemness_and_Therapy_Resistance.
A few months back I had testing done that confirmed my acetylcholinesterase and pseudocholinesterase levels are low, very likely since before my teen years when I started experiencing excessive sweating and post orgasm illness syndrome type symptoms. I was diagnosed with allergies and hyperhidrosis (excessive sweating), but anticholinergics/anhistamines have been a bandaid. I stopped taking them for years and became ill…mood/cognitive/affect/etc. due to a massive buildup of acetylcholine and organophosphates (show in urine testing). Also realized that I have something called post orgasm illness syndrome (symptoms were covered up by the anticholinergics/antihistamines). After orgasm, I get major dark circle/puffy eyes, am irritable, sweaty, anti-social, etc. There’s a clear connect with the defective AChE receptors. Additionally, urine testing showing high levels of organophosphates in my system. Let me know about the testing options as I had blood/plasma draws today and I can still add the antibody testing and remove the cholinesterase testing if need be. I don’t believe I’ve had high exposure to organophosphates lately. I’ve read that galantamine which is a reversible AChE inhibitor is supposed to be helpful in detoxing organophosphates and possibly “reversing” some of the “aged” receptors that were damaged, probably from anesthesia when I was a child. I don’t quite understand why an AChE inhibitor would be helpful if my AChE levels are already low. I have taken benedryl, chlorpheniramine, and hydroxizine in addition to oxybutynin. Recently, the nootropics piracetam, phenylpiracetam, bromantane and sulbuthiamine. Thoughts on how to prevent acetylcholine buildup (other than eating less choline)?
There is also another reason to the complexities here. There is well known study in which C Elegans was found to have diminished span of being when reproduction was a priority. The study was for a small organism that less ability to manage its activity or nutrition differently in response to changes in priorities or outcomes. However, phospholipids are precious, and phospholipids are often utilize to produce essential fluids including reproductive fluids. Cervonic Acid, known as DHA, is an essential antinflammatory component in physiology and is essential in developmental contexts because it allows environmental signals that cause cytokines to be utilize as environmental sensing components instead of eluting inflammatory pathways and cytokines. DHA is a primary enrichment component in Enriched Phosphatidylcholine produced by PEMT, but is also occurs incident to cervix and occurs incident to the emerging fetus, enabling physiology to develop using scarless wound healing instead of inflammatory processes that would produce scabs and scars instead. Scarless wound healing occurs in some experimental organisms. Scarless wound healing also occurs in organisms that regenerate their anatomy after aspect of the anatomy have been remove, such as the Starfish and such as the Axolotl. Some of the organisms can generate the major aspect of their anatomy from the smaller limb, appendage or area. However, the function of PEMT is typically preserved in these organisms.
Similarly, the organs that regenerate themselves in Human anatomy continue exhibition of PEMT function, with coordinated functional interactions between PEMT1 and PEMT2 to enable regeneration.
Thus, reproductive fluids and digestive fluids utilize phosphatidylcholine. Digestive fluids utilize MDR2 to use phosphatidylcholine for digestive fluid synthesis, resulting a requirement for additional choline to be obtained to offset the use of phosphatidylcholine for digestive fluid synthesis.
Thus, the systemic pathology in this instance is likely to include ingestion patterns and reproductive activity that exacerbates a choline deficiency which is being ignored here, but is also ignored globally because it is presumed that abated vital being is required to occur. PEMT pathways reveal, pervasively, the causes of detrimental outcomes but these have ben overtly and in a plainly discernible way excluded from priorities in diagnostics, analyses and therapy. This must change. However, it is essential that patients not be beguiled and tricked into thinking that choline and phosphatidylcholine are detrimental.
make no mistake here. The world seems tumultuous now because since 1841 and 1871, the group of 12, 20 cytokines or conditions which are required for detrimental physiological and detrimental behavioral outcomes, have been excluded from focus, acknowledgment and management by systems of civilization. The 50 factors that interactively shape these 12, or 20 core factors into detrimental outcomes have been allowed to persist in civilizations around the world because they confirm the inaccurate, opiniated, and scientifically refuted as well as statistically refuted concepts and ideologies of the past. Populations are being systematically abrogated and this information shows exactly how it is occurring as well as exactly to alleviate and prevent these nuances of systems from continuing to cause detriment at population levels and from causing detriment to you and those whom you have an interest in assuring exhibit optimal outcomes.
Disease
Every disease requires the exhibition of inflammatory cytokines, 12 or more, and about 20 or more metabolic circumstances as required, essential, causal, correlated and mechanistic links to exhibition of the factors, conditions, behaviors and pathologies know as disease and detrimental behavior. This is well known and presented by the research and data from about every nation upon the Earth and organizations otherwise.
Genetics
Pervasively these cause, enhance or allow genetic anomaly to emerge as changes to metabolic phenotype, thereby causing or enhancing disease and detrimental behavior.
The molecular basis of disease
These cause the exhibition of four major conditions. inhibition of the antinflammatory antihistamine CDP Ethanolamine pathways supply of Phosphatidylethanolmine to the enzyme PEMT. PEMT integrates CH3, which has Hydride the energy that fuels stars, into membrane Phosphatidylethanolamine to produce antinflammatory, enriched, Phosphatidylcholine, thereby causes de novo synthesis of choline and causing enhanced levels of hydride, capacitant/battery function of membranes, and is essential to maintaining background physiological pH between 7.2 and 7.6. This 7.2 to 7.6 background pH is required for conscious cognitive function, awareness or contiguous exhibition of the energy field that is ones being and links ones being to the Universes. PEMT inhibition increases S-Adenosyl Homocysteine, which then becomes Homocysteine, Homocysteic Acid and Homocysteine Thiolactone, thereby promoting systemic dsybiosis and uncoupling of cellular entities from the inclination to participate in group or social function essential to exhibition of an anatomy, as well as promotes exhibition of the enzyme iNOS which potentiates uncoupling of all NOS including iNOS, nNOS and eNOS. Also Resultant of PEMT inhibition, upregulation of P53 and upregulation of Choline Kinase as the first enzyme in the inflammatory histamine(when upregulated) CDP Choline pathway occurs. These impair the physiological basis of social behavior at the cellular level, tissue level, organ level, systemically, in the brain, cognitively and behaviorally.
Inflammatory Cytokine Dysbiosis
Regardless of what factors occur in civilization, such as the nearly perfect quantitative correlation since the 1950s and qualitative correlation since the 1800s between both pollution, chlorine/fluorine in water supply, electricity and wireless communications, use of striate in table salt, these factors cause the most detriment by invoking or perturbation of these 12 or more and 20 or more core group of inflammatory cytokines. These core group of cytokines are shaped interactively into the all of the outcomes observed in civilization, enabled by 50 or more factors that are genetic, molecular, metabolic, systemic, cognitive, behavioral, organizational, systems or civilization level factors. However, these factors must become translated into these 12, 20 or 50 in order to cause the change of such influence into disease or detrimental Human outcomes.
The 12, 20, and 50 factors all interactively, result in increase in Homocysteine derivatives because the 12 and 20 or more factors are potent inhibitors of the enzyme PEMT, although some may also result in upregulation of Homocysteine directly or also cause dysbiosis directly.
Every virus requires the exhibition or manipulation of iNOS for pathology. Every bacteria causes iNOS through membrane Lipopolysaccharide. Choline deficiency causes iNOS because choline deficiency causes massive cellular deterioration in tissues and iNOS increases gaseous pressure in the cytoplasm and plasma membrane interstitial space. iNOS is caused by restraint or entrapment, or forced immobilization, impairing the natural way the influences from all across the universe and from other eras/epochs influence Human behavior and migration. iNOS is caused by wireless communications fields and attenuation from unshielded wired communication. These included wireless mobile devices, wireless home electronics, electronics and even appliances. iNOS is caused by unshielded nonEMF insulated electricity infrastructure, electricity plugins/outlets, conduit, wires, substations, electricity transformers, generators, electronics, etc. iNOS is caused by Chlorine and Fluorine in water. All of these can easily and should have easily been mitigated through shielding, covering, enclosing, mitigating, placing into harmonic multiplexed frequencies/wavelengths, planning, provision of protective shielding and clothing, as well as through building materials selection and implementation of grounded, shielded, insulated conduits, circuit boxes, fuse boxes, wires, plugins, powerstrips, substations, and other factors.
Aging
Aging and the detrimental factors or differential factors correlated with aging, including risk for accidents, dementia, disease and abated being, are 99.99999 resultant of choline deficiency, inhibition of PEMT, inflammatory cytokines, inflammatory cdp choline pathway upregulation, Homocysteine derivatives, uncoupling of iNOS, eNOS, nNOS, as well as factors linked to such uncoupling including reactive molecular species Superoxide, Hydrogen Peroxide, Peroxynitrite, and Hypochlorite which, along with ingestion of meat, chicken, eggs and fish without pro/pre/post Biotics or antibiotics, are potentiators of the number one cause of sudden adverse health events, abated being and detrimental behavior known as trimethylamine-n-oxide. The difference in average span of being between genders are known to be strongly correlated to the difference in average levels of Homocysteine between genders. Every disease can easily be searched for in research literature and the internet along with the word homocysteine or the inflammatory cytokines, revealing that these are implicated in every disease, behavioral health conditions and detrimental behavior.
The Gompertz sigmoid and Makeham Sigmoid, both, when integrated into one, describe statistical graphs of risk for abated being among populations including two curiosities at the beginning and end that are regarded as mysteries, all are perfectly described by Homocysteine levels and more perfectly described by metabolic nuances that effect the metabolic infrastructure the depletes, recycles and prevents increases in Homocysteine.
Therapeutics
A review of therapeutics demonstrated clearly that therapeutics and drugs, including those used in critical and emergency care, caused upregulation of Homocysteine and several single spaced pages describes the effect of Homocysteine as an integral and foundational causes of almost every detrimental factor in disease, impaired biological function, impaired cognition, abated consciousness and discontinuation of vital being. Some even directly cause iNOS.
A useful way to describe this is that Homocysteine increases correlative to age, but modern civilizations and therapeutics as well as wholistic and other capabilities, should be assuring average spans of being between 200 yrs or as being indefinite. However, the baseline levels of Homocysteine and other cytokines are being augmented by Electricity, Wireless Communication, environmental pollution, deficiency, chlorine/fluorine in water, potential of striates in table salt, choline inadequacy, eating meat/chicken/eggs/fish without pro/pre/post biotics or antibiotics, learning which causes double stranded DNA segmentation requiring increased levels of choline, as well as other factors such mineral/vitamin inadequacy and decrease in nutrients within foods.
Each disease increases the level of these cytokines to cause the pathologies linked to such disease. Covid as a disease increases cytokines such as iNOS, resulting in increased levels of these inflammatory cytokines, particularly the 12, 20 or 50 factors. The reason that those who are of increased age and those with other diseases exhibited increased risk, seems to clearly by that their levels of Homocysteine and cytokines were already higher than other populations with less risk. The reason that some of those afflicted by Covid exhibit diverse impairments and pathologies afterward, seems to be that there were underlying existing genetic, metabolic and physiological as well as environmental circumstances that were affecting them more as well as may now be affecting them more than others whom are not experiencing such complications. These factors have to be managed in every patient and every person before they become patients.
Testing of vaccines resulted in adverse or ineffective outcomes among those whom were aged or both aged and in care facilities for the aged. The literature clearly implicates that the reason are not known, but like all of such literature in which causalities are presented as unknown, this is not accurate. Aged exhibits the highest levels of Homocysteine and inflammatory cytokines, on average. Inhibited PEMT and Homocysteine levels, as well as iNOS and other inflammatory cytokines from electricity, wireless communications, chlorine/fluorine, atmospheric/environmental pollution, and striates in table salt, all cause deterioration of the Thymus, hepatic organ, Spleen, and other areas or functions are comprise central nuances of Adaptive, innate, humoral and cellular, as well as other nuances of immunology. These studies and conclusions regarding the vaccine don’t even include acknowledging the metabolic basis of Immunology.
The data and research here provides both high level and specific information about how these factors should have been managed since 1841 and 1878 at the latest. These also demonstrate that these factors are integral to every disease and are not being prioritized adequately, at least since 1878 or perhaps since 1841.
This internet site or portal provides information on how to manage these factors to manage aging, behavior, health and health statuses, including disease.
These clearly show that populations are being systematically caused to exhibit abated vital being and because there has not been found in any civilization a focus on these in care to this instance, although there may be some civilizations that do focus on these factors, this deprivation of Human and civil rights has been utilized to produce bias and cause the outcomes the confirm such bias to occur.
However, there is one civilization that founded its systems upon the Golden incipient nuance of reason known as Life, Liberty and Pursuit of Happiness, which require that the 12, 20 and 50 factors be managed, prevented and alleviated for all whom are among the nation, as well as enabling these benefits to flow among all of Humanity. Regardless of if one considers the founders, constructors and implementers of these imperatives as systems of civilization to be biased or not, it is clear from these three priorities that they either exhibited no such bias, aspired to transcend their own biases if they existed, or aspired to produce a civilization that, itself, was intended to transcend human susceptibility to bias or other impedance to the furtherance of the Human experience.
Not one person whom constructed such systems incipiently are known to exist and not one person whom participated in divergence of civilization’s priorities from these to produce the status quo is known to exist. Thus, there is only the opportunity to get systems back on track in furtherance of Life, Liberty and Pursuit of Happiness among all among the nation, as well as allowing these benefits to flow to Humanity inclusively.
securing information flow and electron flow on web
IPv4 10.15.0.20 10.15.0.20.inaddr.arpa,
this prevents this site from being used to track and mess with contributors to the discussion
an island in the central Pacific Ocean
A vitamin oriented Homocysteine management therapy is available, although it uses the least efficient pathways for homocysteine depletion. http://www.enlyterx.com/ingredients. Enlyte is FDA approved, but it depletes homocysteine through anabolic pathways and that are susceptible to many of the pathologies liked to choline inadequacy. The ingredients and ingredient highlights are here.
All the magnesiums in the ingredients are because it is useful secondary atom in a molecule and because Magenesium readily gives off Molecular Hydrogen which is the foundational atom in material in the Universe.
Zinc and Iron, help in depletion of Dimemthylglycine which accumulates for Betaine/homocysteine depletion by BHMT.
The Folates are not optimal unless the include 6s 5678 Tetrahydrofolate because otherwise dimethylglycine can accumulate and inhibit BHMT depletion of homocysteine. The Methylfolates do potentiate Methionine Synthase depletion of Homocysteine and B12 is provided for mammalian Methionine Synthase function, although this is an anabolic pathway and it can make some cytotoxic oncology therapies less effective as well as it can cause increase in S-Adenosyl Methionine while PEMT function is not being adequately assured. It is very important to manage inhibitors of PEMT otherwise S-Adenosyl Methionine can accumulate and be directed toward pathways which increase Homocysteine.
CoQ10 potentiates quinones and potentially menaquinone(4) which helps depleted Dimethylglycine.
Sodium citrate can supply citrate into the krebs cycle and can provide sodium for Sodium Coupled Choline transporters.
Phosphatidylserine can potentiated Phosphatidylethanolamine if it becomes integrated into membranes. EPA/DHA are also beneficial but DHA supplementation above only menial levels can inhibit PEMT. The levels here are probably alright.
Glycine is used to deplete Glucose metabolites in later aspects of the Glycogen and energy pathways and can be used in biosynthesis. It can also be utilized to help manage Dimethylglycine.
Cysteine is important because provides one of the factors, along with histidine and aspartate that comprise the three molecule location of Cysteine Protease interaction Loci, which when activated causes cellular entities to systemically deterioration without inflammation.
Summarized, the solution omits any of the foundational homocysteine management pathways that the therapeutics industry leaves impaired to cause reliance upon pervasive therapeutics.
https://www.enlyterx.com/ingredients
It continues to be recommended to use danshen/salvia m or Red Sage is recommended to deplete homocysteine through the transsulfuration pathway.
It is recommended to use Selenomethionine, Methylsulfonylmethane and 6s 5678 Tetrahydrofolate to potentiate Trimethylsulfonium and manage dimethylglycine.
It is recommended to obtain dimethlyacetothetine, Trimethylsulfonium, or Trimethylselenonium as well as methylsulfonylmetane and dimethylsulfoxide to potentiate depletion of Homocysteine through Thetin Homocysteine Methylpherase.
It continues to be recommended to use S Methylmethionine sulfonium to deplete homocsyteine through BHMT2 pathway along with zinc, glycine and 6s 5678 tetrahydrofolate to manage dimethylglycine.
Methylthiopurines and Methylethers, both to potentiate Thiopurine S Methyltransferase depletion of Homocysteine.
NAD+ to potentiate S-adenosine homocysteine Hydrolase.
Along with a complete mineral supplement including Diatomic Cationic Metals such as Gold, Copper, Zinc, Magnesium, etc, as well as a complete natural whole food vitamin supplement then support Enlyte in this context.
Using grapeseed, olive oil, or 33 DMB each day, along with 33 dmb or broad spectrum antibiotic during an emergency, along with regular antibiotic (3 routines a year), regular laxative, along with regular pro/pre/postbiotics, help manage trimethylamine-n-oxide and perform as the only known nonmechanical improvement of carotid intima media thickness/plasticity.
It continues to be necessary to comprise the pathways. Phosphatidylethanolamine, Phosphatidylserine, Ca2+, Vitamin D3 activated, phosphatidylcholine, Choline, Cystathionine, tetrahydrobiopterin, L-arginine, L-ornithine, L-citrulline, Superoxide Dismutase, Catalase, N Acetyl L Cysteine, Kolaviron9garcinia Kola seed extract), Curcumin, Berberine.
These then lead to Pregnenolone which is a natural Choline Kinase inhibitor, catabolism of scar tissue and coagulates with serrapeptase and nattokinase. DHEA and Alpha GPC.
Vanadium is important to include in the mineral supplement.
Along with energy protection blankets or covering, covering of energy/power/electrical outlets in dwellings, using emf inhibition stickers and netting for all electronics and devices, only using wireless networks/phones/protocols during an emergency, and removing all of your phone number/address/IP addresses, names, likenesses, and other information from internet site and organizations that have information accessible from communication pathways should really make a difference.
However, drinking only filtered water, eating natural nongmo foods that are as raw as possible, using pink himalayan sea salt instead of any table salt version, as well as daily short duration moderate excercise that includes light resistance, all can comprise a nearly inclusive management of homocysteine.
Increased levels of Catalase can help manage/prevent/alleviate graying hair.
Dimethylacetothetin, Glycolic acid(deriviative of dimethylacetothein) are all found in beauty products. Hyaluronic acid also is found in beauty products but unlike glycolic Acid which cannot be used as a supplement, Hyaluronic Acid and Dimethylaceothetin can be utilized as a supplement. Hyaluronic Acid inhibits leukocyte infiltration of tissues and helps regenerate connective tissue and improve moisture levels in connective tissues.
Implementing these along with Enlyte can result in a remarkable inversion of the aging processes and although refinements may be required or required for optimal achievement, the should assist in elderly, those exhibiting chronic disease, injured, chronic discomfort and pain, advancing disease, and even newly afflicted, as well as those in sudden adverse health event circumstances, all to begin managing outcomes toward 99.999 perception or more optimal outcomes.
These include adequate rest(but not too much). Freedom from atmospheric and environment particulate, decrease in destress, emotional/social stability, all continue enhancing these outcomes.